Teachers & Parents ADHD Resource
ADHD Goes to School: Providing Teachers and Parents with ADHD Specific Management Strategies
by Russell A. Barkley, Ph.D., ABPP
|
||||||
Learning Objectives
This is an intermediate-level course intended to provide mental health professionals with a variety of evidence-based methods for addressing school adjustment issues. After completing this course, mental health professionals will be able to:
- Describe the symptoms and causes of ADHD in children and teens.
- Explain three behavioral methods in the management of ADHD symptoms and associated behavioral and learning problems.
- Discuss four accommodations to the school curriculum and physical environment to reduce the degree of impairment of the student’s functioning.
- List the actions and side effects of three medications prescribed for ADHD.
The materials in this course are based primarily on the book, Managing ADHD in School: The Best Evidence-Based Methods for Teachers, by R. A. Barkley (2016), published by PESI, Eau Claire, WI. It is also based on his more recent book, Treating ADHD in Children and Adolescents: What Every Clinician Needs to Know (2020), Guilford Press. Moreover, recent research was reviewed on best practices for managing ADHD in school settings. This course contains the most accurate information available to the author at the time of this update. The scientific literature on ADHD grows daily, and new information may emerge that supersedes these course materials. This course will equip clinicians to be able to advise parents about, and directly equip educators on, the most effective methods for managing the symptoms of ADHD and associated impairments in children and teens with ADHD in school settings.
Outline
- Introduction
- What is ADHD? Just the Facts
- Symptoms of ADHD
- Demographic Facts about ADHD
- Setting Factors that Influence ADHD Severity
- Causes of ADHD
- General Principles for Managing the Executive Function (EF) Deficits in ADHD
- Externalize Information
- Externally Represent or Remove Gaps in Time
- Externalize Motivation
- Make Problem-Solving Manual
- Intervene at the Point of Performance in Natural Settings
- Approach ADHD and its EF Deficits as a Chronic Condition
- 10 Specific Principles for Managing ADHD
- Classroom Management: Basic Considerations
- Peer Tutoring
- Increasing Incentives and Rewards for Good Behavior and Performance in Your Classroom
- Daily Behavior Report Cards and Behavior Contracts
- Daily Behavior Report Cards
- Behavioral Contracts
- Externalizing Information and Time
- Make Rules Obvious and in Physical Form
- Make Time Obvious or Physical
- Helping Children Improve Self-Awareness
- Transition Planning
- Potential Disciplinary Methods
- Tips for Teen Management
- Medications Used to Manage ADHD
- Types of Stimulants and their Actions
- Side Effects of Stimulants
- Non-stimulants (NERIs: Norepinephrine Reuptake Inhibitors)
- Side Effects of NERI Non-stimulants
- Anti-Hypertensive (Alpha-2) Drugs
- Conclusion
- References and Evidence Base
Introduction
Providing Teachers and Parents with ADHD Specific Management Strategies. Education is the most prevalent domain of impaired major life activities associated with ADHD in children and teens, with more than 90% of those affected having significant problems functioning effectively in this setting. School is also the most seriously impaired domain relative to all other domains such as family, peer, and community functioning. Mental health professionals therefore are routinely called upon to advise families and educators on the most appropriate methods for managing ADHD related symptoms, behavioral problems, and academic performance difficulties in school settings.
What is ADHD? Just the Facts
This section provides a brief review of the symptoms, associated cognitive deficits, demographics, and etiology of Attention Deficit Hyperactivity Disorder (ADHD) as taken from other courses on this website and other sources by Dr. Barkley (on this website for his other books). It is not intended as a substitute for the information in the other courses on this website. Course participants are encouraged to take those other courses for more extensive knowledge about ADHD. The research supporting the information provided below can be found in the other courses by Dr. Barkley as well as in the latest edition of his handbook and clinician’s guide on ADHD.1, 2
ADHD is a neurodevelopmental condition that consists of developmental delays or deficiencies in at least two types of neuropsychological abilities. These two dimensions are inattention and hyperactive-impulsive symptoms.3 The disorder is classified as neuro-developmental because the scientific evidence for the substantial role of neurological and genetic causes in ADHD is now overwhelming and irrefutable (see Causes of ADHD below). ADHD is considered to be neuro-developmental because it is primarily the result of a delay or lag in the development of specific mental abilities. Those deficits are largely due to delays and/or dysfunctioning in the maturation of the brain areas that underlie those abilities. Such brain maldevelopment seems to arise largely from genetics but can also occur as a consequence of damage or other disruptive influences experienced by the child or teen at any time during development, most often during prenatal brain formation.
The symptoms of ADHD are dimensional in that they reflect the extreme end of a continuum of normal or typical human ability in these two areas. Therefore, children and teens with ADHD have a disorder that:
- is beyond their own choice or making;
- is intrinsic to their psychological and physical nature;
- is not a categorical condition, such as being pregnant;
- differs from the behavior and abilities of other students in these dimensions as a matter of degree (quantitative), not as a matter of kind (qualitative);
- will become evident sometime during child development (before 16 years of age in 98% of cases);
- is likely to be pervasive across many, but not necessarily all, situations; and
- is likely to be persistent across development for many, but not necessarily all cases.
Symptoms of ADHD
The general nature of the symptoms most often evident in children and teens with ADHD include:
Inattention:
- Can’t attend well to details
- Makes careless mistakes
- Can’t persist at tasks or sustain attention
- Doesn’t listen
- Doesn’t follow instructions
- Doesn’t finish assigned work
- Is poorly organized
- Avoids or delays starting activities involving sustained effort
- Loses or misplaces necessary items
- Is easily distractible
- Is forgetful
Hyperactivity-Impulsivity:
- Fidgets
- Can’t remain seated
- Runs or climbs inappropriately
- Can’t play quietly
- Often “on the go”
- Talks too much
- Blurts out comments
- Can’t wait
- Interrupts or intrudes
To warrant a diagnosis of ADHD, these symptoms must occur at least often, to a degree that is excessive for the child’s age. The child or teen has to have a majority of the symptoms (six or more) on either list. Several symptoms must have developed in childhood (before 12 years of age). These symptoms must have persisted for at least the past six months, must occur in two or more settings (home, school, work, community), and must lead to impaired functioning in major life activities, such as social (family, peers, community), academic, or occupational activities. Only a small percentage of children will meet all of these conditions, making those who do, more problematic than 92%-95% of the child or adolescent population in these respects.
Deficient Mental Abilities that Contribute to the Symptoms
I and many other clinical researchers conceptualize these symptoms as arising from deficits in the executive functions – such functions permit self-regulation:4
- Goal-directed persistence (attention) and resistance to distraction: What separates the attention problems seen in ADHD from those evident in other disorders, such as depression, is that those with ADHD have problems with sustaining attention to and persisting toward the future. They are less able to persist at getting things done over time, in time, and on a time schedule that involves delayed or future events. Thus, they are able to pay attention to what is happening in the moment, but not to what they need to be doing to be ready for what is coming next or what they have been assigned to do. Even if they try to persist toward tasks or goals, they are more likely than others to react to distractions which are events not relevant to the goal or task. Those distracting events are not just irrelevant things occurring around them, but also irrelevant ideas occurring in their mind. The problem here is not one of detecting those distractors better than others but rather failing to inhibit reacting to those distractors as well as others.
- Remembering to Do (Working memory): A large part of their inattentiveness comes from the inability to hold in mind what goal they have chosen or been assigned, what steps that involves, and monitoring when it has been accomplished. This reflects a deficiency in working memory, which is remembering what to do. Memory for facts, knowledge, or information is not so much the problem as remembering what is to be done and persisting at it until the task is complete or the goal attained. Even if they try to hold in mind the information that is to guide their behavior toward a goal or task, such as instructions or assignments they’ve been given, any distractions will disrupt and degrade this special type of memory. The mental chalkboard of working memory is wiped clean by the distraction, and so the child is now off doing something other than what they are supposed to be doing. And having reacted to a distraction, and so gone “off-task,” they are far less likely to re-engage the original, and now uncompleted, goal or task. In sum, the child or teen with ADHD is less likely than others to remember what they were supposed to be doing. Yes, ADHD children are forgetful. But as you can see here it is a special type of forgetfulness – it is forgetting what they are supposed to be doing (forgetting the goal and the future more generally).
- Inhibition: Children and teens with ADHD are not just impulsive (poorly inhibited) in their actions, which leads them to move around, touch things, and otherwise behave too much (hyperactivity); their deficit in inhibition extends to:
- their verbal behavior (talking excessively) and to their cognitive activities or thinking (impulsive decision-making).
- their self-motivation, meaning that they are more likely than others to opt for immediate rewards or gratification. Put another way, they steeply discount the value of a future or delayed event or consequence (reward or punishment) the further into the future it may occur, causing them to have a high time-preference – they prefer to have small results now rather than larger results later.
- their emotional self-control. They display their emotional reactions more quickly and more likely than do others of their age. And, if strong emotions have been provoked by some event, they will have a far more difficult time moderating or otherwise self-regulating that emotion so as to recover from it in a timely manner. So children with ADHD are less patient, more easily frustrated, quicker to arouse, more excitable, and sillier, yet also more likely to react with anger, and so more likely to respond with aggression when provoked. They show emotions that are less mature and appropriate to the situation and less consistent with or supportive of their future welfare than others. These impulsive emotions differ from those seen in a mood disorder because they are of short duration, provoked, often situation specific, and usually understandable to others, if immature in their expression. Mood disorders are of a much longer duration, not setting specific usually, often unprovoked, and are less or not understandable (rational) to others as to why they may be occurring. They are also more capricious, labile, and extreme.
- Planning and Problem-Solving: ADHD is associated with difficulties in generating multiple possible options for overcoming obstacles encountered when pursuing goals or in contemplating multiple solutions posed by problems. A related deficit is in the ability to construct and execute the steps of a plan necessary to attain a goal. This difficulty is often evident in school settings in handling problems with mental arithmetic, verbal narratives to questions posed in class or on exams, oral reports, written reports, and other tasks in which a complex, well-organized response is necessary.
If you noticed a recurring theme here, it is that ADHD interferes with thoughts, actions, words, motivations, and emotions aimed at organizing behavior across time and preparing for the future instead of just reacting to the moment. To act impulsively, fail to persist, and be distractible is to be nearsighted to the future – to be preoccupied by moments and so be blind to time. The aforementioned cognitive deficits arise from deficits in executive functioning (EF) and so disrupt daily school activities. Therefore, deficient executive functioning in daily life will be evident in problems with:
- Self-Restraint – deficient behavioral inhibition, limited self-control, poor delay of gratification, and difficulties subordinating one’s immediate interests and desires to those of others.
- Self-Management to Time – poor time management and organization across time to achieve one’s goals or accomplish assigned tasks.
- Self-Motivation – an inability to activate and sustain motivation for working on relatively boring, tedious, effortful, or lengthy tasks in which there is no intrinsic interest or immediate payoff.
- Self-Organization and Problem-Solving – difficulty with organizing one’s personal space, desk, locker, academic materials, etc. much less one’s own behavior so as to accomplish work efficiently and effectively. Forgetfulness of what is to be done or what was assigned also occurs, as noted above under working memory. Deficits evident in tasks that require working memory and thoughtful problem solving.
- Self-Regulation of Emotions – difficulty with inhibiting the expression of impulsive emotions in reaction to emotionally provocative events. This is evident in the student being easily excitable, prone to both positive and negative emotional outbursts, and greater-than-typical impatience, frustration, anger, hostility, and reactive aggression.
The vast majority of children and teens meeting research diagnostic criteria for ADHD fall in the bottom 7% of the population in each of these major areas of executive functioning in daily life.5 It is easy to see how such deficits would produce a myriad of difficulties with functioning in educational settings that typically place a premium on these EF abilities.
Demographic Facts about ADHD
- 5%-8% of children and 4%-7% of teens have ADHD (as do 3%-5% of adults, and 2-3% of the elderly).
- Obviously, the prevalence of ADHD therefore declines with age, which implies that some children with ADHD will recover from the disorder by adulthood (estimated to be 10%-34%, depending on one’s definition of recovery). But this decline is also due to some extent to a higher mortality rate (2x) in childhood and even more so in adulthood (nearly 5 x) by mid-life as a result of accidents, suicide, and, in adults, homicide. The disorder has also been recently shown to shorten total life expectancy by as much as 9 to 13 years due to the numerous health and lifestyle problems related to ADHD.
- Hyperactive symptoms decline more steeply with age than do the inattention symptoms. EF symptoms, however, remain more persistent over development and are far more problematic in adulthood than are those of hyperactivity.
- But the number of domains of daily life impaired by ADHD can increase with age because more domains become available for participation than in childhood and those domains involve more EF and self-regulation than do those of childhood (e.g., sex, driving, advanced education, work, managing money, cohabiting with a partner, raising children, etc.)
- In some regions, the prevalence of ADHD may be higher than others, such as in dense urban centers with higher rates of poverty, blue-collar or lower-middle social class neighborhoods, areas surrounding military bases, or regions that have more of the factors that can cause ADHD (toxins, poor prenatal care, more smoking or alcohol use during pregnancy, etc.) than do other regions. (See Causes of ADHD, below.) The reason why ADHD may be more common among the children of certain occupational groups is because more adults with ADHD are likely to be in those occupations. Given the high genetic contribution to ADHD, those adults are more likely to have children with ADHD.
- The sex ratio of ADHD (males to females) ranges 3:1 to 4:1 in children, 2:1 to 2.5:1 in adolescence, and is approximately 1.5:1 in adulthood. The reason for the convergence of the sex differential across development is unknown at this time but recent evidence suggests that ADHD in females is more sensitive to changes in sex hormones like estrogen and progesterone. This in turn suggests a second onset of the disorder in females around the start of their menses, exacerbation of symptoms around their monthly menstruation, and worsening of their EF deficits during peri-menopause.
- The nature of the symptoms of ADHD itself is not different between boys and girls. However, the other disorders or impairments that can coexist with ADHD, such as aggression or depression, may be more or less common depending on the sex of the child. Boys with ADHD may be more likely to have aggressive or antisocial behavior, more likely to engage in risk-taking, and more at risk for later driving problems, drug use and addiction than are girls with ADHD. Girls with ADHD may be more likely to experience peer problems or rejection, depression, anxiety disorders, binge eating pathology or bulimia, and possibly academic failure (though this is arguable) than do boys with the disorder. In both sexes, however, those with ADHD are more prone to all of these coexisting problems than are typical boys or girls.
- There is no evidence of significant or meaningful differences in the prevalence or nature of the disorder across ethnic groups. In some places where an ethnic group may seem to have more ADHD than usual, it is typically because of the other factors noted above that may affect prevalence in a region (i.e., poorer prenatal care and nutrition, higher rates of drug use during pregnancy, higher rates of significant prematurity of babies, etc.). It is not due to some propensity for that ethnic or racial group to have more ADHD due merely to their ethnic or racial background.
- In any given region, a greater or lesser number children may actually be clinically referred and diagnosed with ADHD than the actual prevalence of the disorder within that region. Rates of clinical diagnosis are not the same as rates of true disorder. Some regions have few medical or psychological professionals, have professionals that are less trained in ADHD, have parents and schools that are less knowledgeable or aware of ADHD, or may have few resources for clinical evaluations and treatment of it. There, rates of diagnosis of ADHD may be well below the actual prevalence level for the disorder in that region. In regions with greater economic wealth and hence professional resources, the opposite patterns to those above may occur. That is, rates of diagnosis may match or even exceed the rates of prevalence given above. In upper-income neighborhoods where a premium is placed on academic excellence or acceleration, rates of diagnosis may even be higher than the rates of prevalence; parents (and schools) can pressure doctors to diagnose marginal (or even fictitious) cases of the disorder that don’t meet all the criteria above for having ADHD. This can happen when parents want performance-enhancing medications and/or educational accommodations for their child so they can out-compete other children.6
Setting Factors that Influence ADHD Severity
Children and teens with ADHD may show significant fluctuations in the severity of their symptoms across diverse situations or settings. In general, symptoms of ADHD may often be worse in settings or tasks that:
- are boring or uninteresting;
- involve significantly delayed consequences or infrequent feedback;
- require working independently of others;
- lack supervision;
- involve groups of children;
- are highly familiar (and thus usually less interesting);
- involve parents rather than strangers or less familiar adults;
- include parents or supervisors who talk and reason too much but rarely act to control misbehavior;
- require waiting;
- occur late in the afternoon or evening (due to fatigue in self-control); and
- place substantial restrictions on movement (such as classroom desk work).
All of these settings demand EF and self-regulation. Of course, the symptoms of ADHD can improve in settings that involve factors that are the opposite of those above. Specifically, these best-case situations may involve fun activities, highly stimulating or interesting tasks (e.g., video games), lots of movement (e.g., gym, recess, sports), frequent rewards or feedback, highly supervised settings, working in small teams with peers rather than independently, working one-on-one with an adult, highly novel settings, where supervisors speak briefly but back up their rules quickly with consequences, and where there is little or no pressure to wait for things.
Causes of ADHD
As discussed above, ADHD is known as a neurodevelopmental disorder. That is because its chief causes exist in the broad realms of genetics and neurology rather than in the domain of social causes.
Genetics. ADHD is a highly inherited disorder. For instance, if a parent has the diagnosis, their children are six to eight times more likely to have the disorder (35%-54%). If a child has ADHD, their biological brother or sister is three to five times more likely to have the condition (25%-35%). Their biological mother is three to four times more likely to have ADHD, and their biological father is five to six times more likely to have it. If an identical twin has ADHD, the other twin will be ADHD in 75%-90% of cases. All this clearly shows the genetic (heritable) nature of ADHD.
The degree to which individual differences in genes among people contributes to individual differences in their ADHD symptoms is 65%-80%. In other words, up to 80% of the differences among people in their degree of ADHD symptoms is due to differences in their genetic makeup. This is higher than the genetic contribution to temperament and personality traits, depression, anxiety, antisocial behavior, and even intelligence. It is only slightly less than the genetic contribution to variation among people in their height.
Research currently suggests that there may be as many as 25 to 44 genes involved in causing ADHD. Note that these are not different kinds of genes from those seen in typical people. There is no specific disease gene or genes for ADHD such as may be seen in Tay Sachs or other severe neurological disorders. What is involved in ADHD are different versions of the same genes seen in typical people. For instance, children with ADHD may have a longer version of a gene than that seen in a typical child – this is often known as tandem repeats. For instance, typical children may get four or five copies of a certain gene side-by-side, while children with ADHD may have seven or more copies, thus creating a longer version of this gene. Such variations in gene length and repetition are called polymorphisms. The different version of the gene in cases of ADHD leads to different lengths of proteins and other chemicals, and those lead to different structural changes in the brain. And those differences create differences in the brain’s functioning – sometimes different enough to create ADHD.
This explanation does not mean that all 25 or more risk genes need to have atypical versions in order to create the disorder; only a subset could well cause it. The risk for ADHD increases with the number of risk genes that a child possesses. It also means that cases of ADHD will vary in which genes led to their particular case of the disorder. For instance, as a hypothetical example, it may be that just five to eight genes from among this pool are needed to be different so as to cause a case of ADHD to emerge. But which subset of this risk pool of ADHD genes that differs in any individual case may not be the same subset of genes that caused another case of the disorder. This further means that similar-appearing symptomatic cases of the disorder could still have different underlying genetics for their disorder. Those differences could lead to either subtle or even important differences in the nature of their disorder (some are more impulsive, others more inattentive), in the risks for other disorders (such as depression, learning disorders, smoking or other substance abuse), in the consequences from the disorder (driving impairments, criminal behavior), and even responsiveness to different ADHD medications or other treatments.
Understanding the genetics of ADHD also helps us to understand why ADHD may be more likely to be affiliated with some other psychiatric disorders, as they may share the same or similar underlying genes. Some of the risk genes for ADHD, for instance, have been found in reading disorders, autistic spectrum disorders, and bipolar disorder, while other genes are shared with oppositional defiant disorder, conduct disorder, and even nicotine dependence and alcoholism.
Because ADHD is a disorder that falls along a continuum or dimension, and because it is inherited, one can see signs of an ADHD phenotype within a family having the genetic form of the disorder. That is to say that parents and siblings of a child with ADHD may be more likely to manifest some milder forms of the symptoms or traits of the disorder even if they don’t meet all of the requirements for receiving a diagnosis of it. [Note: the same is true in autistic spectrum disorder, which is also strongly genetically influenced.]
While most cases of ADHD are genetic and involve inheritance of the genes contributing to ADHD from parent to child, new cases of ADHD can arise in a family due to genetic mutations in ADHD-risk genes that occur in the parent’s eggs or sperm. These mutations get passed along to the children, creating a new line of ADHD risk in the family even though the parents do not have the risk genes for the disorder in their own blood or other cells (except their gametes).
Neurology. Hundreds of research studies employing a variety of methods for measuring brain structure, functioning, development, and connectedness (networks) now support the conclusion that ADHD is largely a neurologically caused disorder. At least five to six brain regions are reliably linked to the disorder. These brain regions can be seen in Figure 1, below. They are the prefrontal cortex, the anterior cingulate cortex (at the midline of the frontal lobes), the frontal section of the corpus callosum (the splenium), the basal ganglia, and the cerebellum (mostly the central vermis region). Less certain is whether or not the thalamus and amygdala are involved. Interestingly, evidence suggests that the right side of the brain in some or most of these regions may be somewhat more involved in creating ADHD than the left. But both sides of these regions appear to be involved in the disorder. In general, the brains of children and teens with ADHD are about 3%-10% smaller globally in gray matter volume (the material on the outside layer of the brain). But these five specific brain regions appear to be even smaller – about 15%-30% smaller than normal for age.
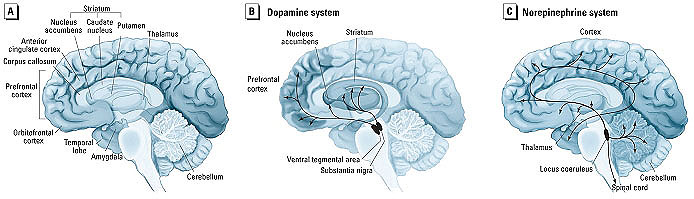
Figure 1. (A) Diagram of the human brain - regions involved in ADHD are the prefrontal cortex, anterior cingulate cortex, striatum, cerebellum, and corpus callosum (splenium or anterior aspect). (B) The dopamine system of the brain – a neurotransmitter system influenced by certain ADHD medications. (C) The norepinephrine system of the brain – a neurotransmitter system affected by other ADHD medications. From ehp.niehs.nih.gov.
Research demonstrates that these regions are functionally interconnected to form one of the seven major brain networks – the executive system. In my view, that system underlies the human capacity for self-regulation and, as Fuster concluded, for the cross-temporal organization of behavior toward goals (future-oriented action). There are at least four or five subnetworks in the executive network, each of them associated with different parts of the brain, that can help us understand how executive functions help us self-regulate—or, in the case of ADHD, make it difficult to do so:
- The Inhibitory Executive Network: Think of this subnetwork as allowing us to resist responding to goal-irrelevant events, or distraction. It's responsible for the voluntary inhibition of ongoing behavior and emotions, as well as the suppression of competing responses to goal-irrelevant events, both internal and external.
- The "What" or Cold Executive Network: Essentially, this network allows what we think about (mainly imagery and self-talk) to guide what we do. It also permits the higher-level function of the manipulation of goal-related mental representations (analysis and synthesis, or mental play) so as to support planning and problem solving.
- The "When" (Timing) Executive Network: When we choose to act can be as or more critical to the success of a plan than what we had planned to do, and it's this subnetwork that gives us a subjective sense of time and the temporal sequencing of thought and action as well as the timeliness in executing such actions.
- The Hot (Emotional) or "Why" Executive Network: This is probably the subnetwork that makes the final decisions about goal choices and the selection of planned actions to attain them. But it also permits the top-down regulation of emotion in the service of those goals and our longer-term welfare, probably through the use of self-imagery and self-talk, or the working memory network above.
You may be wondering where hyperactivity fits into the executive function neuroanatomy picture of ADHD. In part it certainly arises from defective functioning of the inhibitory network. But in addition to the subnetworks listed above is the motor activity regulation network. Disturbances in this network are thought to also give rise to the hyperactive symptoms of the disorder.
Developmental research finds the brain to be two to three years delayed on average in its development in these regions, especially the prefrontal lobes, and to be 10%-30% less active than in typical comparison cases. More recently, fine-grained neuro-imaging methods have revealed defective microstructures in the subcortical (white matter) neural networks that connect these brain regions to each other. These methods make the maturational deficiencies in ADHD even more obvious in the interconnectedness (networks) of these structures than was evident in studies of just surface gray matter. While the size of the entire brain may eventually become closer to normal with age, the connectedness and functioning of the neural networks is likely to remain deficient and highly variable into adulthood for many cases, though not for all cases. There is no doubt now that ADHD is of neurologic origin, hence its classification as a neurodevelopmental disorder.
You can now understand why ADHD is both genetic and neurological. The genes involved in causing ADHD are genes that build and operate certain regions and networks in the brain during development. Different versions of genes involved in ADHD compared to typical people result in differences and even deficiencies in these structures, connectedness, and their functioning. ADHD is therefore a neuro-genetic disorder in many cases.
But ADHD can also arise from non-genetic sources, as shown in Figure 2 below. Most of these are conditions or factors that can potentially interfere with brain growth and functioning, especially in the ADHD-related brain regions mentioned above. For example, it is now known that when a mother drinks alcohol beyond a certain amount during her pregnancy, they increase the risk for ADHD in her unborn child two to three times greater than the typical risk (Fetal Alcohol Exposure in Figure 2). This is likely the result of these substances having a toxic effect on brain development. Other pregnancy complications may do much the same, abnormally altering brain development. These include conditions such as the number of maternal infections during pregnancy, delivery complications (Perinatal hazards in Figure 2), degree to which the baby was born substantially premature (Low Birth Weight in Figure 2), degree of severe stress to which the mother was exposed during pregnancy, extent of abuse of other drugs alcohol during pregnancy, and other factors. A smaller percentage of ADHD cases may be due to brain damage suffered after the child is born. This can include diseases, brain trauma, tumors, stroke, or even poisoning, such as with lead or pesticide exposure (Lead and Post-Natal Damage in Figure 2).
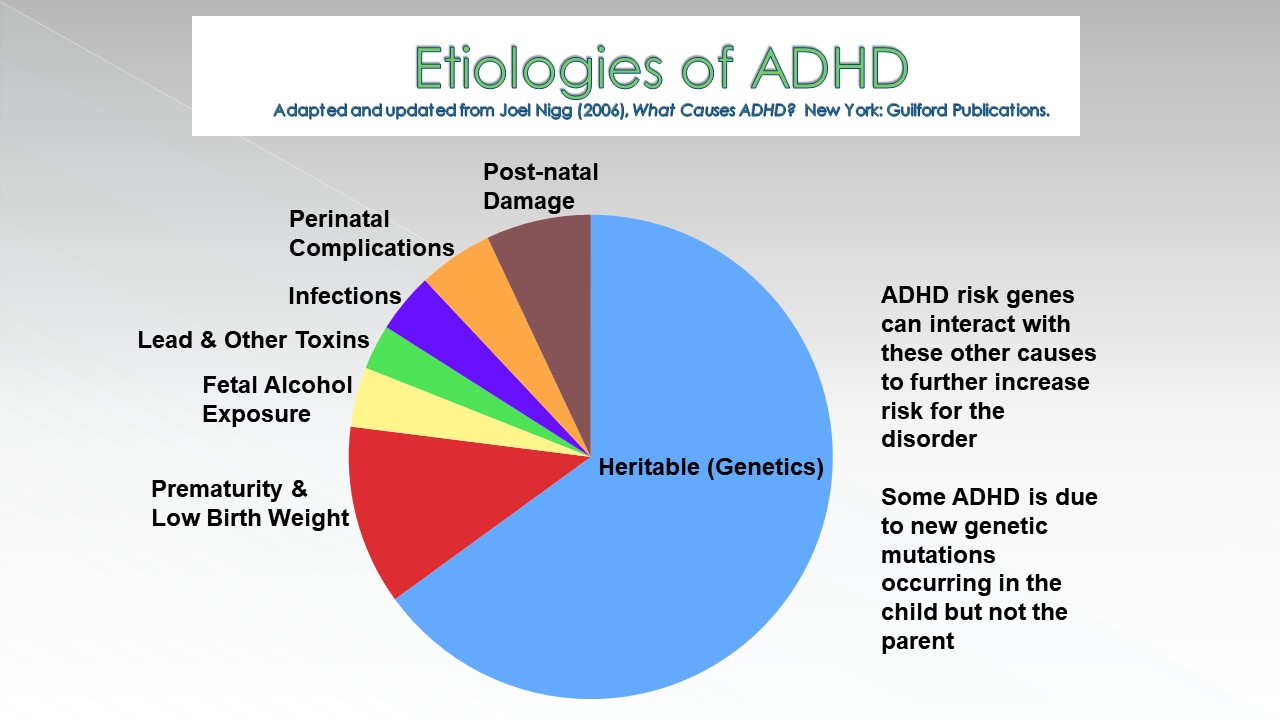
Figure 2. Etiologies of ADHD
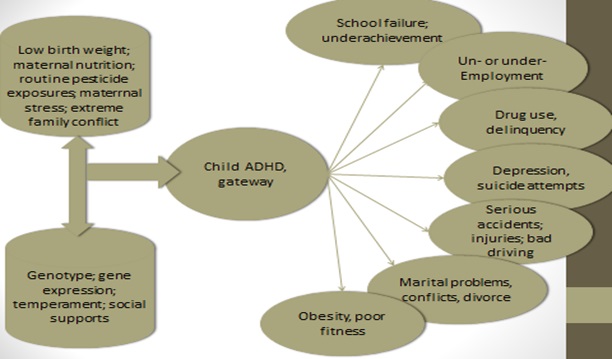
Most recently, some research shows that these environmental risk factors can interact with the ADHD risk genes discussed above to further heighten a child’s risk for ADHD. This is illustrated in Figure 3. For instance, if a mother passes one of the major ADHD risk genes to her child and she smokes during that pregnancy, the risk for ADHD in her child is magnified two to three times greater than would have been the case from either the risk gene or maternal smoking alone (evidence of a risk gene by environmental interaction). In summary, about 60%-70% of cases of ADHD are likely due to inheritance or genetic factors. Another 20%-25% arise from pregnancy complications that may adversely affect brain development or that interact with ADHD risk genes to do so. The remaining 5%-10% may arise from injuries to the brain sustained after birth.
Notice here that there is no compelling evidence that social factors, such as parenting or educational environment, have been found to cause ADHD. The degree of evidence against such explanations is now so compelling that no reputable scientist working in this field gives them any credence at this time. This does not mean that social factors are unimportant; just that they are not important in explaining the initial causes of ADHD. They are still important in determining how impaired someone with ADHD will be in specific situations. Social factors are also important in influencing what the risk to a child will be for other psychiatric disorders known to be due in part to these social factors (anxiety, depression, oppositional behavior, conduct disorder, etc.). And surely you will recognize that social environmental factors determine how much access to care children get for treating their ADHD, and the quality of that care, including in the school setting.
.
Research has now ruled out the likelihood that dietary substances such as sugar or food preservatives and additives cause ADHD. However, some children may be sensitive to food colorings enough to induce or mildly worsen their ADHD symptoms. But such effects are found in a minority of children and often when they are preschoolers, not when they are teens or adults. Anti-oxidants have not been found to be linked to ADHD and thus taking food supplements that increase them in the body seem unlikely at this time to benefit children with ADHD. Iron deficiencies have been found in some studies in children with ADHD but this finding is not reliable across studies and it is not clear that iron supplements would be helpful for management of the disorder in these cases. ADHD does not arise from watching TV excessively, using computers too frequently, or playing video games. Although the degree of TV viewing in the early preschool years was correlated to a small degree with inattention in some studies, other studies completely failed to replicate that finding. And the direction of causation is also unclear here. We know that children with ADHD like to watch TV more than typical children so ADHD could be leading to more TV viewing. The disorder is certainly associated with increased use of the Internet or video games, social media, and other screen-based technology, but these don’t cause ADHD, rather ADHD predisposes children to excessive electronic media use. For instance, children with short attention spans would rather play a fast-paced exciting video game than read for pleasure; they would rather watch TV than exercise; they would rather use the Internet or social media on their smartphones to socialize with others, even strangers, than interact in person with neighborhood or school-based peers.
As you can see from the above review, ADHD is a neurodevelopmental disorder of attention, inhibition, and executive functioning that largely arises from neurological and genetic origins.
General Principles for Managing the Executive Function (EF) Deficits in ADHD
As noted above, children and teens with ADHD have serious deficits in their executive functioning and self-regulation. In dealing with these deficits, there are several basic principles that must be kept in mind in constructing specific interventions for the educational problems of these individuals. Here are the principles that underlie the effective management of ADHD-related EF deficits in the schools.7
Externalize Information
If the process of regulating behavior via internally represented forms of information (e.g. working memory or the internalization of self-directed behavior) is impaired or delayed in those with ADHD and EF deficits, then those students will be best assisted by “externalizing” those forms of information. The provision of physical representations of such information will be needed within the school setting at the point of performance. Since covert or private information is weak as a source of stimulus control, making that information overt and public may assist with the strengthening of control of behavior via that information. Make the information physical and place the physically represented information outside of the child just as it was in earlier development. Internal forms of information generated by the executive system, if they have been generated at all, appear to be extraordinarily weak in their ability to control and sustain behavior toward the future in those with EF deficits. That behavior remains largely under the control of the salient aspects of the immediate context. So, make the information external again.
The solution to this problem is not to nag those with ADHD-related EF difficulties to simply try harder or remember what they are supposed to be working on or toward. Instead, the solution is to fill the immediate context with physical cues comparable to the internal counterparts that are proving ineffective. In a sense, clinicians treating those with EF deficits must beat the environment at its own game. Whenever possible, minimize sources of high-appealing distractors that may subvert, distort, or disrupt task-directed mentally represented information and the behavior it is guiding. In their place should be cues, prompts, and other forms of information that are just as salient and appealing, yet are directly associated with or are an inherent part of the task to be accomplished. Such externalized information serves to cue the individual to do what they know.
If the rules that are understood to be operative during educational or occupational activities, for instance, do not seem to be controlling the child‘s behavior, they should be externalized. They can be externalized by posting signs about the school environment and its rules and having the student frequently refer to them. Having the student verbally self-state these rules aloud before and during individual work performances may also be helpful. One can also record these reminders on a digital recorder that the student listens to through an earphone while working.Externally Represent or Remove Gaps in Time

Figure 4. Time Escapes Children with ADHD
The organization of an individual’s behavior both within and across time is one of the ultimate disabilities rendered by ADHD. EF deficits create problems with time, timing, and timeliness of behavior such that they are to time what nearsightedness is to spatial vision. They create a temporal myopia in which the individual’s behavior is governed even more than normal by events close to or within the temporal now and the immediate context rather than by internal information that pertains to longer term, future events. This helps us to understand why students with EF deficits make the decisions they do, short-sighted as they seem to be to others around them. If one has little regard for future events, then much of one’s behavior will be aimed at maximizing the immediate rewards and escaping from immediate hardships or aversive circumstances, without concern for the delayed consequences of those actions. Those with deficient EF could be assisted by making time itself more externally represented, by reducing or eliminating gaps in time among the components of a behavioral contingency (event, response, outcome). Caregivers and others can also help to bridge such temporal gaps related to future events.
Another solution is to reduce or eliminate the problematic time-related elements of a task when feasible. The elements should be made more contiguous. Rather than telling the child that a project must be done over the next few days, week, or month, assist them with doing a step a day toward that eventual goal so that when the deadline arrives, the work has been done, but done in small daily work periods with immediate feedback and incentives for doing so.
Externalize Motivation
The EF theory of ADHD also hypothesizes that a deficit will exist in the internally generated and represented forms of motivation needed to drive goal-directed behavior. Complaining to these children about their lack of motivation (laziness), drive, will power, or self-discipline will not suffice to correct the problem. Pulling back from assisting them to let the longer-term natural consequences occur, as if this will teach them a lesson that will correct their behavior, is likewise a recipe for disaster. Instead, artificial means of creating external sources of motivation must be arranged at the point of performance in the context in which the work or behavior is desired.
For instance, the provision of artificial rewards, such as tokens, may be needed throughout the performance of a task or other goal-directed behavior when there is little or no immediate consequences associated with that performance. Such artificial reward programs become for the person with ADHD-related EF deficits what prosthetic devices are to the physically disabled, allowing them to perform more effectively in some tasks and settings with which they otherwise would have considerable difficulty. The motivational disability created by EF deficits makes such motivational prostheses essential for most children deficient in EF.
The methods of behavior modification are particularly well suited to achieving these ends. Many techniques exist within this form of treatment that can be applied to children with ADHD related EF deficits. What first needs to be recognized is that (1) internalized, self-generated forms of motivation are weak at initiating and sustaining goal-directed behavior; (2) externalized sources of motivation, often artificial, must be arranged within the context at the point of performance; and (3) these compensatory, prosthetic forms of motivation must be sustained for long periods. If the external motivation is removed, the behavior will not be further sustained and the individual will regress to more erratic goal-directed behavior with less ability to sustain actions toward tasks and goals.
In general, there are two reasons to do behavior management for anyone: for informational training and for motivational sustaining. The former is done for individuals who have not yet acquired a skill. Once the skill is taught through behavioral or other pedagogical methods, those methods can be withdrawn and the behavior sustained presumably by contact with the natural contingencies. But in EF disorders such as ADHD, the issue is not ignorance or lack of knowledge of a skill; the problems are with the skill’s timing and execution at key points of performance and with the self-motivation needed to sustain the performance. Behavioral treatments can provide the motivational or behavior-sustaining assistance needed. Removing the external motivation after improvement in task performance will result in a loss of motivation and a return to the baseline state of limited self-motivation and an inability to sustain actions toward goals.
By equating EF with self-regulation (SR), the EF theory of ADHD (via Gross’ modal model of emotional self-regulation) illustrates at least five vectors through which EF/SR can influence goal-directed activities:
- situation selection
- situation modification
- attentional control/redirection
- re-appraisal
- response modification/suppression
In attempting to assist students in rehabilitating or at least compensating for their EF deficits, these five vectors offer opportunities in which clinicians can strive to improve such deficits. While this can be done by directly working with the student, it is likely to be greatly assisted by advising caregivers to assist the individual with these five pathways of SR. Modifying the “point of performance,” as further discussed below, readily fits into the situation modification vector of SR. Various cognitive behavioral therapies may prove useful at the re-appraisal pathway. The point here is not to map out all possible ways by which these five vectors of SR could be used to boost EF in those with EF deficits, but to make clinicians cognizant that such pathways are available.
Related to this idea of motivational deficits accompanying EF disorders such as ADHD is the literature on self-regulatory strength and the resource pool of effort (will power) associated with activities of SR. As nicely summarized by Bauer and Baumeister (2011),8 research indicates that each implementation of EF (working memory, inhibition, planning, reasoning, problem-solving, etc.) may deplete this limited resource pool temporarily such that protracted use of EF may greatly deplete the available pool of effort. This can result in students being less capable of SR (EF) in immediately succeeding time periods. They are thus more likely to experience problems or fail outright in their efforts at EF/SR and their resistance to immediate gratification. Such temporary depletions may be further exacerbated by stress, alcohol or other drug use, illness, or even low levels of blood glucose. More recently, debate has centered around whether this view of EF/SR is a limited resource pool or not. Until that is resolved, it seems useful for clinicians to view it as such and try not to overtax EF for extended time periods in those with ADHD while also providing frequent opportunities to restore or replenish it.
Research also indicates what factors may serve to more rapidly replenish the resource pool. These include:
- routine physical exercise,
- taking 10 minute breaks periodically during SR strenuous situations,
- relaxing or meditating for at least three minutes after such SR exerting activities,
- visualizing the rewards or outcomes while involved in EF/SR tasks,
- arranging for periodic small rewards throughout the tasks for SR-demanding settings,
- engaging in self-affirming statements of self-efficacy prior to and during such tasks,
- generating positive emotions, and
- consuming light but frequent doses of glucose-rich beverages during the task (arguable).
Some research further suggests that the actual capacity of the resource pool may be boosted by routine physical exercise and by routine practicing of tasks involving self-regulation daily for two weeks.
Make Problem-Solving Manual
Children with ADHD cannot hold information in mind or manipulate mental information as well as other children. That means that mental problem-solving is difficult for them. To assist them, try to think of ways to make the problem, or parts of the problem, physical in various ways so that the child can manipulate the parts of the problem manually to facilitate mentally held information. For instance, if they have mental arithmetic to do, let them have some marbles, a number line, an abacus, or some other way to physically count and manipulate the information to help them solve the math problems. If the child has a written essay to do, encourage them to use 3x5 file cards and to write a different idea on each card as the ideas come to mind. Just have them think and free associate to the assigned topic. As each idea is stated, have them write it down on a separate card. Now the child can take these “idea cards” and reorganize them into a possible essay on that topic. I am sure you can think of other ways to do this for a child or teen with ADHD. Remember, it’s not the method, but the principle that should be emphasized here: make solving problems manual work and not just mental work.
Intervene at the Point of Performance in Natural Settings
Given the above principles, clinicians should likely reject most approaches to intervention for students with ADHD related EF deficits that do not involve helping them with an active intervention at the point of performance. Once-per-week tutoring is unlikely to succeed in helping to manage the student with deficient EF without efforts to insert accommodations at key points of performance in natural settings to address the impaired domains of educational activities. This is not to say that extensive training or retraining of EF, as with working memory training, may not have some short-term benefits. Such practice has been shown to increase the likelihood of using working memory and of boosting the SR resource pool capacity in normal individuals, at least temporarily (Bauer & Baumeister, 2011), and chiefly on highly similar tasks. What is missing is evidence of far transfer – that is, of improvements in behavior and functioning in natural settings and on dissimilar tasks involving that same EF component.
Approach ADHD and its EF Deficits as a Chronic Condition
The foregoing review of the etiologies of ADHD lead to a much more general implication: The approach taken to its management must be the same as that taken in the management of other chronic medical or psychiatric disabilities. Diabetes is an analogous condition to many forms of EF deficits. At the time of diagnosis of diabetes, all involved must realize that there is currently no cure for the condition. Still, multiple means of treatment can provide symptomatic relief from the deleterious effects of the condition, including taking daily doses of medication and changing settings, tasks, and lifestyles. Immediately following diagnosis, the clinician works to educate the patient and family on the nature of the chronic disorder, and then designs and implements a treatment package for the condition. This package must be maintained over long periods to maintain the symptomatic relief that the treatments initially achieve. Ideally, the treatment package, so maintained, will reduce or eliminate the secondary adverse consequences of leaving the condition unmanaged. However, each patient is different and so is each instance of the chronic condition being treated. As a result, symptom breakthroughs and crises are likely to occur periodically over the course of treatment that may demand re-intervention or the design and implementation of modified or entirely new treatment packages. Changes to the environment that may assist those with the disorder are not viewed as somehow correcting earlier faulty learning or leading to permanent improvements that can permit the treatments to be withdrawn. Instead, the more appropriate view of psychological treatment for ADHD is one of designing a prosthetic educational environment that allows the student to better cope with and compensate for the disorder going forward. Behavioral and other technologies used to assist people with ADHD related EF deficits are akin to artificial limbs, hearing aids, wheel chairs, ramps, and other prostheses that reduce the handicapping impact of a disability and thus allow the individual greater access to and better performance of their major life activities. Those methods do not eliminate the disorder; instead, they provide the additional social and cultural scaffolding around the student with EF deficits so that performance in that specific setting can be more effective.
10 Specific Principles for Managing ADHD
Based on the principles reviewed in the previous section for addressing EF deficits in children and teens with ADHD, one can develop 10 specific rules that need to be followed in setting up any program to address those deficits. Others rules can be found in my recent book, 12 Principles for Raising a Child or Teen with ADHD (2021, Guilford Press). The 10 most appropriate for educators are:
- Rules and instructions provided to children with ADHD must be clear, brief, and often delivered through more visible and external modes of presentation than is required for the management of normal children. Stating directions clearly, having the child repeat them out loud, having the child utter them softly to themselves while following through on the instruction, and displaying sets of rules or rule-prompts (e.g. stop signs, big eyes, big ears for “stop, look, and listen” reminders) prominently throughout the classroom are essential to proper management of ADHD children. Relying on the child’s recollection of the rules as well as upon purely verbal reminders is often ineffective.
- Represent time and time periods externally (physically). Children with ADHD are less capable of using their sense of time to manage their current behavior and get work done in time, over time, and on time. When short time intervals of an hour or less are required to do work, then represent that time period using a clock, kitchen timer, counting device or other external means to show the child how much time they have left and how quickly it is passing. The large (1-ft.) clock at addwarehouse.com can serve this purpose. Or just use a spring-loaded kitchen cooking-timer placed on the child’s desk. For longer time periods, break the work down into shorter periods with smaller work quotas and allow the child to take frequent breaks between these shorter work periods.
- Consequences used to manage the behavior of ADHD children must be delivered swiftly and more immediately than is needed for normal children. Delays in consequences greatly degrade their efficacy for children with ADHD. As will be noted throughout this chapter, the timing and strategic application of consequences with children with ADHD must be more systematic and is far more crucial to their management than for normal children. This is not just true for rewards, but is especially so for punishment, which can be kept mild and still effective by delivering it as quickly upon the misbehavior as possible. Swift, not harsh, justice is the essence of effective punishment.
- Consequences must be delivered more frequently, not just more immediately, to children with ADHD in view of their motivational deficits. Behavioral tracking, or the ongoing adherence to rules after the rule has been stated and compliance initiated, appears to be problematic for children with ADHD. Frequent feedback or consequences for rule adherence seem helpful in maintaining appropriate degrees of tracking to rules over time.
- The type of consequences used with children with ADHD must often be of a higher magnitude, or more powerful, than that needed to manage the behavior of normal children. The relative insensitivity of children with ADHD to response consequences dictates that the methods chosen for inclusion in a behavior management program must have sufficient reinforcement value or magnitude to motivate children with ADHD to perform the desired behaviors. Suffice it to say, then, that mere occasional praise or reprimands are simply not enough to effectively manage children with ADHD.
- An appropriate and often richer degree of incentives must be provided within a setting or task to reinforce appropriate behavior before punishment can be implemented. This means that punishment must remain within a relative balance with rewards or it is unlikely to succeed. It is therefore imperative that powerful reinforcement programs be established first and instituted over one to two weeks before implementing punishment in order for the punishment, sparingly used, to be maximally effective. Often children with ADHD will not improve with the use of response cost or time out if the availability of reinforcement is low in the classroom and hence removal from it is unlikely to be punitive. “Positives before negatives” is the order of the day with children with ADHD. When punishment fails, this is the first area that clinicians, consultations, or educators should explore for problems before instituting higher magnitude or more frequent punishment programs.
- Those reinforcers or particular rewards which are employed must be changed or rotated more frequently with ADHD than normal children given the penchant of the former for more rapid habituation or satiation to response consequences, apparently rewards in particular. This means that even though a particular reinforcer seems to be effective for the moment in motivating child compliance, it is likely that it will lose its reinforcement value more rapidly than normal over time. Reward menus in classes, such as those used to back up token systems, must therefore be changed periodically, say every two to three weeks, to maintain the power of efficacy of the program in motivating appropriate child behavior. Failure to do so is likely to result in the loss of power of the reward program and the premature abandonment of token technologies based on the false assumption that they simply will not work any longer. Token systems can be maintained over an entire school year with minimal loss of power in the program provided that the reinforcers are changed frequently to accommodate this problem of habituation. Such rewards can be returned later to the program once they have been set aside for a while, often with the result that their reinforcement value appears to have been improved by their temporary absence or unavailability.
- Anticipation is the key with children with ADHD. This means that teachers must be more mindful of planning ahead in managing children with this disorder, particularly during phases of transition across activities or classes, to insure that the children are cognizant of any shift in rules (or consequences) that is about to occur. It is useful for teachers to take a moment to prompt a child to recall the rules of conduct in the upcoming situation, repeat them orally, and recall what the rewards and punishments will be in the impending situation before entering that activity or situation. Think ahead, think aloud is the important message to educators here. By themselves, such cognitive self-instructions are unlikely to be of lasting benefit, but when combined with contingency management procedures, they can be of considerable aid to the classroom management of ADHD children.
- Children with ADHD must be held more publicly accountable more often for their behavior and goal-attainment than normal children. The weaknesses in executive functioning associated with ADHD result in a child whose behavior is less regulated by internal information (mental representations) and less monitored via self-awareness than is the case in normal children. Addressing such weaknesses requires that the child with ADHD be provided with more external cues about performance demands at key points of performance in the school, be monitored more closely by teachers, and be provided with consequences more often across the school day for behavioral control and goal attainment than would be the case in normal children.
- Behavioral interventions, while successful, only work while they are being implemented and, even then, require continued monitoring and modification over time for maximal effectiveness. One common scenario is that a student responds initially to a well-tailored program, but then over time, the response deteriorates; in other cases, a behavioral program may fail to modify the behavior at all. This does not mean behavioral programs do not work. Rather, such difficulties signal that the program needs to be modified. It is likely that one of several common problems occurred (e.g., rewards lost their value, program was not implemented consistently, program was not based on a functional analysis of the factors related to the problem behavior).
Classroom Management: Basic Considerations
Consider the recommendations throughout the remainder of this book as you would a food buffet – choose from among these various methods those you find most suitable for the child or teen with ADHD you have in mind to help. I begin with some basic features of the classroom and teaching style that can help improve the school functioning of children and teens with ADHD. In reviewing these, keep in mind an important distinction between proactive and reactive teaching methods. Many suggestions below are examples of proactive teaching and behavior management. They are in contrast to the customary reactive approach many teachers take with ADHD students. Here, a change is made to a classroom situation or the curriculum or a plan is set up in advance of any problem occurrence. It is done in order to reduce the likelihood of such problems happening in upcoming situations. Proactive teaching also increases the probability that appropriate behavior and school performance are likely to occur. After reading, you will likely agree that proactive methods are superior to reactive methods in dealing with students with ADHD as the former actually reduces or even prevents the likelihood that a problem will arise in a situation. The latter only deals with it after it has occurred.
- Have a school psychologist or master teacher who is knowledgeable in ADHD and school management methods serve as a liaison or consultant to other teachers in the school who have ADHD children in their classrooms.9 This consultant can provide basic information about ADHD to the teacher (such as that presented in earlier sections) as well as make recommendations for specific classroom accommodations and behavior management strategies, such as those described in the remainder of this course.
- Don’t retain a child in grade! Research shows that this is associated with multiple harms and few if any benefits. Develop a real treatment plan instead of repeating a failure.10
- Use the first few weeks of the school year to establish behavioral control of the classroom. Focus more on establishing clear rules and providing swift and reliable consequences for them. Give less emphasis to the curriculum or lesson plan and place more effort into establishing behavior management. Then you can gradually shift the emphasis to the content of the lesson plan.
- Decrease the child or teen’s total workload to what is essential to be done rather than what is merely “busy work” assigned to fill class time. Ask yourself, “How much work does this student need to do to demonstrate that they have acquired the concept I am teaching?” That should be enough.
- Give smaller quotas of work at a time with frequent breaks (i.e., five problems at a time, not 30, with short breaks between work episodes). For instance, take the worksheet of 30 math problems you want done and cut off the top row of five problems. Hand this snippet of work to the child to be done within the next few minutes. When they complete the work and bring it to you, then cut off the next row of five problems and assign that work to them to be done within a few minutes. Continue this process until all of the problems are done. The principle to follow here is to assign smaller quotas of work at any one time, give a break, then assign another small quota. This makes the work fit within the child’s attention span and so is more likely to get done.
- Use traditional desk arrangement in the classroom (all desks face forward to the teaching area).
- Seat the child with ADHD close to the teaching area to permit more supervision of and interaction with the child. It also provides you the capacity to engage in more frequent accountability of the child to you for their conduct and performance.
- Target productivity (number of problems attempted) first and accuracy second. Start first by rewarding the child for each problem attempted and ignore the accuracy for the time being. Once productivity has improved, you can then increase your focus on the accuracy of the work being done. But if you focus on accuracy first (right or wrong), you will not encourage and may even punish productivity if you mark a few problems wrong.
- Don’t send unfinished classwork home for parents to do. Parents of ADHD children have enough stress at home with the ordinary home responsibilities and school homework to be done and do not need to be over-burdened with a teacher’s failed responsibility. Unfinished classwork shows that the problem lies at school, within the classroom. And that is precisely where solutions are to be implemented and not shirked.
- Give out homework assignments weekly so parents can plan their week accordingly.
- Reduce/eliminate homework for elementary children (research is arguable that it benefits students until high school).11 If homework is to be given, keep it to 10 minutes total x the child’s grade level in school (e.g., 10 minutes x third grade = 30 minutes total).
- Allow some restlessness at the child’s work area or desk as long as child is working. Try letting the child squeeze a stress ball (rubber ball) in their left hand while they are working or let the child sit on a balance or exercise ball instead of a chair. This ball allows some movement to maintain stability while seated and can help the child concentrate on their work.12
- Give frequent but brief breaks for physical exercise throughout the school day.
- Get color-coded binders and other commercial organizing systems to help keep student materials and assignments better organized.
- Try letting students do color-coding of text that is to be read using highlighters for marking key points in the text. Then have the child write these highlighted key points down on paper after the reading is done.
- Use participatory teaching: give the student something useful and physically active to do to help you while teaching. This can be having the student stand next to you and hold the pointer while they point to material on the blackboard that you are currently discussing with the class. Or it can be having the student write key words or math problems down on the blackboard as you discuss that material.
- Let students practice skills drills on computers – let students use learning software programs to rehearse skills that have just been covered in the class. Research shows that children with ADHD pay more attention to computer software learning programs and learn more from the practice with them than they do when working on mimeographed work sheets.13
- Discourage impulsive answers to questions. Try using laminated work slates (white boards) about 1 ft. x 1 ft. in size. Each child gets a small white board and marker and when questions are asked, everyone writes the answer on their board and holds it up in the air. Then you call on someone only after ALL boards are up. That student can then explain to the class how they got that correct answer.
- Assign a homework “study-buddy.” This is like peer tutoring (discussed below) but done outside of school. Have children living near each other from the same class do their homework together alternating whose home they meet at to do so.
- Alternate low-appeal with high-appeal activities within your classroom to maintain the children’s interest level. Too many boring topics or activities back to back lead a child with ADHD to lose focus, become distracted, and therefore become disruptive to your class.
- Be more animated, theatrical, and dramatic when you teach. (Make it interesting!) Be like Robin Williams in the movie, The Dead Poets Society, not like Ben Stein in Ferris Bueller’s Day Off. If you are not enthusiastic or very interested in what you are teaching, then don’t expect the student with ADHD to be interested in it either.
- Touch a child lightly when talking to them to get their undivided attention. This also signals to the child that what you are about to say is important. So when you have something to say to the student with ADHD, go to them, place your hand on the child’s hand, arm, or shoulder, and say what you need to say. But keep it brief – get to the point quickly or you will lose their attention.
- Schedule the most difficult subjects in the first few periods of the school day when the student’s attention span is at its maximum. Leave the more active and entertaining subjects for a later time of the day.
- Use direct instruction, programmed learning, or highly structured or regimented teaching materials that have short assignments, clear goals, and frequent quizzes to provide feedback to the ADHD student for demonstrating mastery of the material.
- Have the child pre-state their work goals. Ask her, “How many problems can you do for me in the next five minutes?” Children with ADHD are more likely to do an assignment they have chosen then one imposed on them by another. After they complete it, if you want more work done, then ask them how many more problems they can do for you. Again, the concept here is to give brief periods of work interspersed with brief breaks so as to refresh the student’s short attention span.
- Train the student in keyboarding and word processor skills as early as possible. This is because students with ADHD have a high occurrence of fine motor coordination problems and difficulties with handwriting. So don’t tax their deficits in motor control so much and give the student alternative means of expressing their ideas in print.
- Give the student with ADHD after-school help sessions, extra tutoring, books on tape, and videos to reinforce the classwork you have assigned. When they stay after school to meet with you, you can then assist that child as well with homework completion.
- Require continuous note-taking during lectures and while the child is reading assigned material. The child with ADHD should be taking brief notes of key points in what they are reading, viewing, or listening so as to help focus and sustain their attention to the work. Again, permit some movement while they are concentrating. This not only reduces ADHD symptoms but it can help to improve their poor working memory.
- Suggest to parents that they consider combining the behavioral interventions discussed throughout this book with ADHD medications to maximize the benefits of both.14
Peer Tutoring
Evidence clearly demonstrates that when students with ADHD work in dyads with their peers in order to learn new material, they are more likely to concentrate and to learn that material more quickly than if they just listen to a classroom lecture. This is known as peer tutoring.15 It essentially involves the following brief steps:
- Create, discuss and distribute scripts (work sheets based on the concept or skill you are teaching).
- Teach any new concepts and skills to class as you normally would.
- Provide initial instructions for the work that is to be done.
- Break the class up into dyads (pairs).
- Have one student in each dyad be the “tutor.” That student is to teach the other student in the pair what it was the teacher just taught in their lecture and what is contained on the worksheet. This student-tutor then quizzes their partner on the material.
- You should move around or circulate in the classroom during this time, supervising behavior, and coaching the dyads as needed.
- Be sure to alternate who plays the tutor/student roles in the dyad for the next task or assignment.
- Re-organize the class into new dyads daily or weekly so that the same children are not working together in the same pair for too long.
- Graph or post quiz results on a bulletin board at the front of the class.
Increasing Incentives and Rewards for Good Behavior and Performance in Your Classroom
As noted in previous sections, students with ADHD have far less self-motivation than do other students, meaning they will not be able to persist for as long as others in doing work for which there is no immediate reward or consequence. It was shown that to help make up for this intrinsic motivation deficit, teachers need to provide more “external’ or artificial consequences to students with ADHD when work is to be done. Here we present numerous ways to do this:
- Increase your use of verbal praise, approval, appreciation and other forms of positive feedback for the ADHD student’s good behavior and work performance.
- Be a one-minute manager (Lots of short episodes of praise throughout the class period). For several decades, one of the best-selling business management books has been The One Minute Manager by Kenneth H. Blanchard. The essence of this book was that the best managers who had the best relations with employees and received the most work from those employees were those who did the following actions: They spent only as much time in their office as was essential. They spent far more time periodically circulating among their staff. When they did, the supervisor would just take one minute with an employee, notice anything good, useful, productive, or otherwise positive that the employee had done, commented briefly on this and how much that work was appreciated, and in other ways showed that they valued this employee. They made sure that the comments were accurate statements of what the employee had done and that the appreciation being shown was realistic. They understood that excessive and cloying praise would not be well received, but brief, accurate statements of recognition for work well done and realistic appreciation for that work will be well-accepted and result in greater future motivation by this employee to contribute further to the workplace productivity. Then the supervisor moved on to another employee and did the same. Teachers should do the same with their students, but especially with those who have ADHD.
- Use a token or point system to organize privileges and their price.16 Token economy management systems provide students with “tokens,” known as secondary reinforcers, when students demonstrate a specific target behavior. The steps for setting up a token economy reinforcement system are:
- Decide on the goals to be met (for example, completion of independent seat-work).
- Decide on the type of token to be used (for example, poker chips, tiddlywink chips, stickers, check marks on a card at the student’s desk).
- Decide how many tokens are to be earned by demonstrating each particular target behavior (teachers can break more complex tasks down into component parts and give tokens for each part completed).
- Student and teacher together work out the types of activities and other privileges that the tokens could be exchanged for (e.g., five tokens equals five minutes of free time at a classroom computer or iPad). Create a written menu of these activities and their associated costs and post this menu in a visible place near the student.
- Students are taught the value of the tokens (model what has to happen to earn a token and explain what the tokens can be exchanged for within the available classroom toys, games, and other activities).
- Students can exchange tokens for activities on a daily basis. Don’t delay the exchange beyond a day. And the more frequent the exchange takes place during the day, the more motivating the tokens are likely to be.
- The system should be monitored to assess its effectiveness – does it work? Are there increases in appropriate target behaviors?
- Teachers usually have limited or no budgets for buying toys, games, computers, and other privileges for their classroom. To address this problem, get parents to send in old games/toys to upgrade the class supply of fun activities. You can do this at the beginning of the school year by sending home a memo to parents asking them to clean out their closets, cabinets, basements, etc. of any older toys that their child no longer uses. Instead of donating these to Goodwill Stores, as parents often do, give them to the school. The donations are tax deductible. Send the memo out again after the Christmas school break and you are likely to get another load of toys, games, etc. to help bolster the available rewards you have in your classroom.
- Get video games donated to the class for use during free time and make it one of the privileges to be earned through the class point system. Many families have older versions of Game Boys, X-Boxes, Play Stations, and other gaming devices that their children may no longer be using, having upgraded to the latest models. But these video games are still fun to play and can be motivating to other students in the classroom as rewards for getting work done and earning the necessary tokens to get that privilege.
- Try using team-based (group) activities and associated rewards. This capitalizes on the fun of team competitions to learn and get work done. Break your class up into teams of four to five students per team. The members of the teams are to work together to complete a project or assignment. The teams compete against other teams in getting work done and striving to earn tokens or other rewarding activities. Team members are likely to help keep each other focused and on-task and provide beneficial structure and encouragement to the student with ADHD on that team.
- Try creating (or buying) a tone-tape for use with a self-reward program (you can buy these recordings at the addwarehouse.com website).
- Create an audio digital recording that is composed of tones, such as a bell ringing, a buzzer sounding, a piano key, or any other sound. These sounds are recorded so that the time gaps between them are unpredictable. This creates a variable interval frequency schedule of tones. For the first recording, make the tones occur frequently but keep the brief intervals between the tones unpredictable or random.
- This recording is to be used when students have work to do at their desks.
- When you are ready to use this recording, tell the class that you are turning on a recording of some sounds. They will hear these sounds while they are working. Now, when a tone sounds while they are doing desk work, the students are to self-evaluate by asking themselves if they were working (on task) or not when the sound was heard. The students are to then give themselves a point if they were working when the tone sounded. If they were off task, they must deduct a point from their scorecards. Students can use + and – signs on the card to indicate this. When the work is completed, the students can add up how many tokens they earned (pluses) and this is how many they have to spend on various activities in the token system discussed above.
- Use the Attention Training System – this is a small, automated box for dispensing frequent rewards to ADHD children during work periods (see Figure 5, below).17 The box has a digital display panel on the front that shows how many points a student has earned. There is a red light on the top of the box and a buzzer inside the box. When the student starts working at their desk, the device is turned on. The box will give the student a point per minute. The teacher carries a small wireless transmitter. If they see the student off-task or otherwise not working, they presses a button on this transmitter. A red light flashes on the box, the buzzer sounds, and a point is subtracted off of the total points shown on the digital display. In short, the box delivers the rewards at a frequent pace while the teacher periodically removes points if the student gets off-task. After the work period ends, the student can use these points to buy privileges in the classroom token system discussed above.

Figure 5. Attention Training System (Gordon Systems, Syracuse, NY)
Daily Behavior Report Cards and Behavior Contracts
Two of the most effective tools for helping to improve the behavior and school performance of children with ADHD are daily behavior report cards, also known as note-home cards, and behavior contracts. Both are additional methods of proactive teaching and behavior management first addressed above in Classroom Management: Basic Considerations.
Daily Behavior Report Cards
Any behavior recording system, or report card, must be set up according to certain rules if it is to be maximally effective.
- Daily goals must be stated in a positive manner.
- The card specifies both behavioral and academic goals.\
- The targets are to be a small number of goals.
- The teacher provides quantitative feedback – usually a numerical rating or grade.
- The feedback is provided at the end of each class period.
- There is to be regular daily communication with parents (the card goes home each school day for review by the parents).
- Consequences are established at home and are tied to the student’s school behavior and performance. Parents essentially set up a home token system in which a list of privileges is created and a point value or cost is assigned to each. The tokens or points earned from the daily report cards are to be spent for these privileges.
- Solicit parental cooperation before starting.
- Get student input into the goals especially with older children and teens.
- Review the card weekly for any necessary modifications.
The boxes below contain instructions that can be shared with parents about a daily behavior report card, how to implement it, and the kinds of cards teachers and parents can create for use with a student with ADHD.
|
Parent-teacher Handout for Using a Daily School Behavior Report Card |
|
A daily school behavior report card involves having the teacher send home an evaluation of your child’s behavior in school that day, which can be used by you to give or take away rewards available at home. These cards have been shown to be effective in modifying a wide range of problems with children at school. Due to their convenience and cost effectiveness and the fact that they involve both the teacher(s) and parents, they are often one of the first interventions you should try if behavior problems at school are occurring with your child. The teacher reports can consist of either a note or a more formal report card. We recommend the use of a formal behavior report card like those shown at the end of this handout. The card should list the “target” behavior(s) that are to be the focus of the program on the left-hand side of the card. Across the top should be numbered columns that correspond to each class period at school. The teacher gives a number rating reflecting how well the child did for each of these behaviors for each class period. Some examples are provided at the end of this handout. How the Daily Report Card WorksUsing this system, teacher reports are typically sent home on a daily basis. As the child’s behavior improves, the daily reports can be reduced to twice weekly (Wednesdays and Fridays), once weekly, or even monthly, and finally phased out altogether. A variety of daily report cards may be developed and tailored for your child. Some of the behaviors targeted for the program may include both social conduct (shares, plays well with peers, follows rules) and academic performance (completes math or reading assignments). Targeting low academic performance (poor production of work) may be especially effective. Examples of behaviors to target include completing all (or a specified portion of) work, staying in the assigned seat, following teacher directions, and playing cooperatively with others. Negative behaviors (e.g., aggression, destruction, calling out) may also be included as target behaviors to be reduced by the program. In addition to targeting class performance, homework may be included. Children sometimes have difficulty remembering to bring homework assignments home. They may also complete their homework but forget to return the completed work to school the next day. Each of these areas may be targeted in a school behavior report card program. It is recommended that the number of target behaviors you work on be kept to about four or five. Start out by focusing on just a few behaviors you wish to change, to help maximize your child’s success in the program. When these behaviors are going well, you can add a few more problem behaviors as targets for change. We recommend including at least one or two positive behaviors that the child is currently doing well with, so that the child will be able to earn some points during the beginning of the program. Typically, children are monitored throughout the school day. However, to be successful with problem behaviors that occur very frequently, you may want to have the child initially rated for only a portion of the school day, such as for one or two subjects or classes. As the child’s behavior improves, the card can be expanded gradually to include more periods/subjects until the child is being monitored throughout the day. In cases where children attend several different classes taught by different teachers, the program may involve some or all of the teachers, depending on the need for help in each of the classes. When more than one teacher is included in the program, a single report card may include space for all teachers to rate the child. Alternatively, different report cards may be used for each class and organized in a notebook for children to carry between classes. Again, the card shown at the end of this handout can be helpful because it has columns that can be used to rate the child by the same teacher at the end of each subject, or by different teachers. The success of the program depends on a clear, consistent method for translating the teacher’s reports into consequences at home. One advantage of school behavior report cards is that a wide variety of consequences can be used. At a minimum, praise and positive attention should be provided at home whenever a child does well that day at school, as shown on the report card. With many children, however, tangible rewards or token programs are often necessary. For example, a positive note home may translate into television time, a special snack, or a later bedtime. A token system may also be used in which a child earns points for positive behavior ratings and loses points for negative ratings. Both daily rewards (e.g., time with parent, special dessert, television time) and weekly rewards (e.g., movie, dinner at a restaurant, special outing) may be included in the program. Advantages of the Daily Report CardOverall, daily school behavior report cards can be as or even more effective than classroom-based behavior management programs, with effectiveness increased when combined with classroom-based programs. Daily reports seem particularly well suited for children because the children often benefit from the more frequent feedback than is usually provided at school. These programs also give parents more frequent feedback than would normally be provided by the child. As you know, most children, when asked how their school day went, give you a one-word answer, “Fine,” which may not be accurate. These report card programs also can remind parents when to reward a child’s behavior, and forewarn parents when behavior is becoming a problem at school and will require more intensive work. In addition, the type and quality of rewards available in the home are usually far more extensive than those available in the classroom, a factor that may be critical with children who need more powerful rewards. Aside from these benefits, daily school report cards generally require much less time and effort from your child’s teacher than do classroom-based programs. As a result, teachers who have been unable to start a classroom management program may be far more likely to cooperate with a daily report card that comes from home. Despite the impressive success of report card programs, the effectiveness of the program depends on the teacher accurately evaluating the child’s behavior. It also hinges on the fair and consistent use of consequences at home. In some cases, children may attempt to undercut the system by failing to bring home a report. They may forge a teacher’s signature or fail to get a certain teacher’s signature. To discourage these practices, missing notes or signatures should be treated the same way as a “bad” report (i.e., child fails to earn points or is fined by losing privileges or points). The child may even be grounded for the day (no privileges) for not bringing the card home. Some Examples of Daily School Report CardsSeveral types of school behavior report cards that rely on daily school behavior ratings will be discussed here. Two examples are provided at the end of this handout. These are the cards we recommend most parents use if they want to start a school behavior report card quickly. One card is for classroom behavior, the other is for recess behavior. Use whichever card is most appropriate for the problems your child is having at school. Two sets of each card are provided so that you can make photocopies of that page and then cut the page in half to make double the number of cards. Notice that each card contains five areas of potential behavior problems that children may experience. For the class behavior report card, columns are provided for up to seven different teachers to rate the child in these areas of behavior or for one teacher to rate the child many times across the school day. We have found that the more frequent the ratings, the more effective is the feedback for the children and the more informative the program is to you. The teacher initials the bottom of the column after rating the child’s performance during that class period to ensure against forgery. If getting the correct homework assignment home is a problem for some children, the teacher can require the child to copy the homework for that class period on the back of the card before completing the ratings for that period. In this way, the teacher merely checks the back of the card for the child’s accuracy in copying the assignment and then completes the ratings on the front of the card. For particularly negative ratings, we also encourage teachers to provide a brief explanation to you as to what resulted in that negative mark. The teachers rate the children using a 5-point system (1 = excellent, 2 = good, 3 = fair, 4 = poor, and 5 = very poor). The child takes a new card to school each day. These can be kept at school and a new card given out each morning, or you can provide the card as your child leaves for school, whichever is most likely to be done consistently. As soon as the child returns home, you should immediately inspect the card, discuss the positive ratings first with your child, and then proceed to a neutral, businesslike (not angry!) discussion with your child about any negative marks and the reason for them. Your child should then be asked to formulate a plan for how to avoid getting a negative mark tomorrow. You are to remind your child of this plan the next morning before your child departs for school. After the child formulates the plan, you should award your child points for each rating on the card and deduct points for each negative mark. For instance, a young elementary school aged child may receive five chips for a 1, three for a 2, and one chip for a 3, while being fined three chips for a 4 and five chips for a 5 on the card. For older children, the points might be 25, 15, 5, –15, and –25, respectively, for marks 1–5 on the card. The chips or points are then added up, the fines are subtracted, and the child may then spend what is left of these chips on the privileges on the home reward menu. Another daily report card program is provided for dealing with behavior problems and getting along with others during school recess periods or free time periods each day. Again, two cards are provided on the page so that you can make photocopies of the page and cut the pages in half to double the number of cards. The card is to be completed by the teacher on recess duty during each recess or free time period. It is inspected by the class teacher when the child returns to the classroom, and then should be sent home for use, as above, in a home chip/point system. The classroom teacher should also be instructed to use a “think aloud–think ahead” procedure with the child just prior to the child’s going out for recess or free time. In this procedure, the teacher (1) reviews the rules for proper recess behavior with the child and notes that they are written on the card, (2) reminds the child that he/she is being watched by the teacher on recess duty, and (3) directs the child to give the card immediately to the recess monitor so the monitor can evaluate the child’s behavior during recess or free time. As these cards illustrate, virtually any child behavior can be the target for treatment using behavior report cards. If the cards shown here are not suited for your child’s behavior problems at school, then design a new card with the assistance of your therapist, using the blank cards provided at the end of this handout. They do not take long to construct and can be very helpful in improving a child’s school behavior and performance. From Barkley, R. A. Defiant Children: A Clinician’s Manual for Parent Training. Copyright 1997 by The Guilford Publications. |
|
Daily School Behavior Report Card
|
|||||||
|
Child’s Name________________________________________________________ Date________ Teachers: Please rate this child’s behavior today in the areas listed below. Use a separate column for each subject or class period. Use the following ratings: 1 = excellent, 2 = good, 3 = fair, 4 = poor, and 5 = very poor. Then initial the box at the bottom of your column. Add any comments about the child’s behavior today on the back of this card. |
|||||||
| Class periods/subjects: |
1
|
2
|
3
|
4
|
5
|
6
|
7
|
| Behaviors to be rated: | |||||||
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
| Teacher’s initials: |
___
|
___
|
___
|
___
|
___
|
___
|
___
|
| Place comments below or on back of card | |||||||
| From Barkley, R. A. Defiant Children: A Clinician’s Manual for Parent Training. Copyright 1997 by The Guilford Publications. | |||||||
|
Daily Recess and Free Time Behavior Report Card |
|||||||
|
Child’s Name________________________________________________________ Date________ Teachers: Please rate this child’s behavior today during recess or other free time periods in the areas listed below. Use a separate column for each recess/free time period. Use the following ratings: 1 = excellent, 2 = good, 3 = fair, 4 = poor, and 5 = very poor. Then initial at the bottom of the column. Add any comments on the back. |
|||||||
| Class periods/subjects: |
1
|
2
|
3
|
4
|
5
|
6
|
7
|
| Behaviors to be rated: | |||||||
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
| Teacher’s initials: |
___
|
___
|
___
|
___
|
___
|
___
|
___
|
| Place comments below or on back of card | |||||||
| From Barkley, R. A. Defiant Children: A Clinician’s Manual for Parent Training. Copyright 1997 by The Guilford Publications. | |||||||
|
Daily School Behavior Report Card
|
||||||||
|
Child’s Name________________________________________________________ Date________ Teachers: Please rate this child’s behavior today in the areas listed below. Use a separate column for each subject or class period. Use the following ratings: 1 = excellent, 2 = good, 3 = fair, 4 = poor, and 5 = very poor. Then initial the box at the bottom of your column. Add any comments about the child’s behavior today on the back of this card. |
||||||||
| Class periods/subjects: |
1
|
2
|
3
|
4
|
5
|
6
|
7
|
|
| Behaviors to be rated: | ||||||||
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
|
|
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
| Teacher’s initials: |
___
|
___
|
___
|
___
|
___
|
___
|
___
|
|
| Place comments below or on back of card | ||||||||
|
||||||||
Behavioral Contracts
Instead of a behavior report card, teachers can set up an in-class behavior contract.18 These contracts should contain the following elements:
- Set forth academic work and behavioral goals explicitly and clearly in a written form, for instance:
- I (the student) agree to complete all of my written math and language arts work with at least 80% accuracy.
- I will remain quiet, follow directions, and listen.
- Explicitly specify rewards to be earned, for example:
- 15 extra minutes of playtime at end of school day
- Access to special “reserved” toys or play activities
- Use of class computer for play or work for 15 extra minutes
- Receive 10 points for every task completed accurately
- Help my teacher by completing some errands or in-class jobs
- If I have a successful week, I will earn a special activity with my parents.
- Specify punishment explicitly, for example:
- Loss of 10 points or tokens for each task not completed
- Five sheets of “do a task” in time out
Externalizing Information and Time
Recall from the above discussion of EF deficits that children and teens with ADHD have very poor working memory. That means that they cannot hold as much information in mind or for as long as other students. They are also less likely to call up such information from memory and keep it consciously in mind when they are entering class periods or during a change in a situation from a prior activity to the next or to a new one. Since “internal” or mental information is not very effective at guiding an ADHD student’s behavior, it is helpful to boost working memory by placing key pieces of information in the student’s visual or other sensory fields in that work location. Putting such information in a physical form in the visual field of the student is called “externalizing” the key information and cues. This section briefly reviews some ways that teachers can help “externalize” critical pieces of information about the situation and any time intervals that may be important for that situation, class, or work period. This is another example of a form of proactive teaching and behavior management.
Make Rules Obvious and in Physical Form
- Post rules on posters at the front of the class – you can post different sets of rules for each type of work period.
- Create a three-sided stop sign from poster board. Each side is a different color and each contains the rules for one of three different situations. For instance:
- Use: red = for lecture time, yellow = for desk work, green = for free play
- When the new situation starts, call the class to attention, then rotate the sign to the appropriate color and rules for the appropriate situation, then have students read these rules out loud in unison.
- Place laminated color-coded card sets on the student’s desk such that each card contains a set of rules for each subject or class activity. When that activity starts, direct students to turn their card deck to the appropriate set of rules for that activity. Each activity has different rules and a different color card to make it easier to identify. Have the child state the rules on that card at the start of each activity.
- Encourage the child to use soft vocal self-instruction during work. The child talks to themselves periodically while working, saying out loud in a soft voice the instructions they are to follow. Or, they can softly read aloud the rules on the card for that work period, as discussed above.
- Make sure you are giving your commands and instructions to a child in an effective manner. Here are some key points to keep in mind to help you do so:19
- Make sure you mean it! That is, never give a command that you do not intend to see followed up to its completion. When you make a request, plan on backing it up with appropriate consequences, either positive or negative, to show that you mean what you have said.
- Do not present the command as a question or favor. State the command simply, directly, and in a businesslike tone of voice.
- Do not give too many commands at once. Most children are able to follow only one or two instructions at a time. To start, try giving only one specific instruction at a time. If a task you want your child to do is complicated, then break it down into smaller steps and give only one step at a time.
- Make sure the child is paying attention to you. Be sure that you have eye contact with the child. If necessary, go to the child, touch their shoulder, or gently turn the child’s face toward yours to ensure that he/she is listening and watching when the command is given.
- Reduce all distractions before giving the command. This is a very common mistake that teachers make. Often, teachers try to give instructions while a student is engaged in some competing activity, usually something fun. You cannot expect children to attend to you when something more entertaining is going on in the room. Either turn off or terminate these distractions yourself or tell the child to turn them off before giving the command.
- Ask the child to repeat the command. This need not be done with each request, but can be done if you are not sure the child heard or understood the command. Also, for children with a short attention span, having them repeat the command appears to increase the likelihood they will follow it through.
- Create task cards. If your student is old enough to have tasks to do about the classroom, then you may find it useful to create a chore or task card for each job. Or, as I noted above, you can create cards containing the rules for particular subjects you are teaching, such as reading time, math time, etc. Each card can be a different color to further signal that the rules during this subject are different from those for other subjects. This subject card or task card can simply be a 3x5 file card. Listed on it are the steps involved in correctly doing that task or for that subject period. Then, when the child is to begin that task or subject, simply hand the child the card and state that this is what you want done. Of course, this is only for children who are old enough to read. These cards can greatly reduce the amount of arguing that occurs about whether a child has done a job or chore properly or obeyed the rules for a particular class period. You might also indicate on the card how much time the task should take to be completed and then set a kitchen timer for this time period and place it on the child’s desk or at their work station so the child knows exactly when it is to be done.
- Create “nag tapes” This is a digitally recorded set of encouragements recorded by Dad or Mom (or the teacher) with reminders of the rules for on-task behavior. The child can listen to this recording using ear buds during schoolwork.
Make Time Obvious or Physical
As noted in a previous chapter, children and teens with ADHD cannot manage or guide their behavior based on their sense of time. So teachers should not rely on a child’s subjective sense of time, which is impaired in children with ADHD. As suggested earlier, “externalize” time. Essentially, this means using some external timekeeping device in the child’s workspace to help children with ADHD see how much time they have to do something, and then how much of it has passed and how much is left as they complete their work. To do this, you can use clocks, timers, watches, recorded time signals, etc., anything to show how much time they have to do an assignment. For example, you can use the Time Timer,20 which is a timer device that is an 8 in. x 8 in. clock with a red dial that signals a time period of up to one hour (see Figures 6 and 7). When a child has deskwork to do within a set time period, you can set this clock to that time period. The time available shows up in red on the clock face and as time passes, the amount of red exposed decreases until time us up and a signal sounds to indicate the end of the work period.

Figure 6. Time Timer
Of course, digital timers can also be found on the Internet, such as the My Time Activity Timer.21

Figure 7. My Time Activity Timer
You can also download a variety of online stopwatches and timer apps for a tablet, iPad, or smartphone at: online-stopwatch.com/classroom-timers. These include traditional clock faces, time bombs, cartoon characters running races, virtual hourglasses, etc.
Helping Children Improve Self-Awareness
As you learned above, children and teens with ADHD are less aware of their own behavior than are typical students because they do not monitor their ongoing behavior as well or as often as do those other students. Research does not show any definitive means by which teachers can improve the self-awareness or self-monitoring of students with ADHD. But here are some methods that have been used by clinical researchers and others to try to do so.22
- Have the child record their work productivity on a daily chart or graph. Put this graph on public display, such as on a bulletin board at the front of the class. Each day the student records how many problems they completed in a particular class period on this graph or chart. This is done so the student can see how well they are performing in class over time.
- Go back and look at the daily behavior report cards above. You can easily see that these could be cards that are completed by the child instead of the teacher at the end of each class period. In other words, the child provides a self-evaluation of their behavior and performance in the areas specified on the card. This can be done using the same rating scale that the teacher was using to rate or grade the child’s behavior. The child rates themselves on this daily conduct card and the teacher checks it to see if they agree with the child’s self-evaluation. If not, the teacher discusses this difference of opinion and why they would disagree with the child. Then the child can re-rate the card based on this new feedback. Teachers are encouraged to start with a standard behavior report card (as described in a previous section) that they complete. Then, after a few weeks, when the child’s behavior seems to have improved, the teacher can transition over to this type of self-evaluation.
- For young children, researchers have developed a simpler cueing system for letting children know that they may be behaving inappropriately and to stop and self-monitor their current actions. For instance, the teacher cues a young child to immediately stop and self-monitor by saying the word “Turtle.” The child has been previously instructed that when they hear the teacher say that word to them, they are to:
- Stop what they are doing, pull in their hands and arms to their sides, and legs close together.
- Slowly look about the classroom to regain their sense of where they are and what is happening.
- The child asks themself out loud, “What was I told to do?”
- Then the child is to give the answer and return to the assigned task, or follow the instruction that they were given.
- For successfully doing so, some teachers have given children small ink-stamp impressions on their hand using an ink-stamp containing the picture of a turtle. The child collects these stamps on the back of their hand throughout the day. These turtle stamps then are used like tokens to purchase special privileges in class later that day. Or the teacher can substitute turtle stickers that are glued to a card kept on the child’s desk. If those sorts of stickers cannot be purchased, then the teacher can simply give the student a token, like a poker chip, for each successful act of self-monitoring.
- Use a device called the MotivAider. The MotivAider23 – is a small vibrating box with a built-in digital timer (see Figure 8). This small box is worn by the child on a belt or placed in a pocket. It is a tactile cueing device that vibrates at intervals set by the teacher. These intervals can be fixed (i.e., every minute) or they can be set to be random. Set the timer so the box periodically cues the child with a vibration stimulus that means it is time to self-monitor what they are doing or to pay attention to the assigned work.
Figure 8. MotivAider
- For older children or teens with ADHD, it is recommended to use nonverbal confidential cues to signal the teen to stop and self-monitor their current actions. You can do this by telling the teen beforehand that when they see you show this signal, they are to self-evaluate what they are doing and get back to work, get back to following a given instruction, or just settle down and regain behavioral control if that is the issue. For example, you can say to the student that if you drop a paper clip by their desk, it was no accident. For her, it’s a cue to self-evaluate, regain control, or otherwise pay attention to the teacher.
- In more severe cases of ADHD, you or a school psychologist can consider video recording the child during a particular troublesome class period. Afterward, during a scheduled time for this purpose later that same day, the student and you or the psychologist can review the recording with the child, stopping the video periodically to discuss what the child was doing correctly or incorrectly at certain key moments. Then discuss what the child could be doing differently if there was a problem noted. It is recommended that this method be paired with some type of reward system, such as a token system, to reward the student for both the review period (when you go over the video with them) and for improvements they subsequently make in their class behavior.
Transition Planning
Children and teens with ADHD, as noted previously, have trouble not only with working memory (remembering the rules that apply in a given situation) but also with self-monitoring of their own behavior. Both of these problems conspire along with their inattentiveness to pose frequent problems when the student is transitioning from one activity, class period, or classroom to the next one on their daily schedule. As a result, problem behaviors can often occur during or just after such transitions. To help address this situation, it is recommended to use a method called transition planning. This is to be discussed with the child before it is put into use. Essentially, here is what the student is to do BEFORE starting a new activity, class subject, or even entering a new classroom:
- Before the child enters a new situation (next class, recess, going to lunch room) have them STOP!
- The teacher then reviews two or three rules the child needs to obey in this new situation.
- The child then repeats those rules back, out loud.
- The teacher explains what the incentive or reward is to be in that situation for obeying those rules (tokens, time on the computer, extra play time, etc.).
- The teacher then establishes with the child what the punishment is to be if a rule is broken.
- The teacher then assigns the child an immediate instruction to do or activity to start. For instance, the teacher can say “Go to your desk, get out your math book, and turn to chapter X and start reading.”
- The child then enters the new situation, and follows your plan.
- The teacher is to reward the student frequently throughout the new activity.
- At the end of that situation, the teacher speaks briefly with the student to evaluate their success (or failure).
A teacher can also augment or replace this procedure with a 3x5 in. file card on which are written the rules the child is to follow routinely when entering this new situation, class subject, or classroom. That way, the child has the “externalized” rules written on the card to take with them to keep in view on their desk throughout the period.
Too often, teachers allow students to go through these transitions unassisted. Then when problems develop, the teachers are forced to react to this situation, usually with discipline. The proactive behavior management outlined above is far superior to reactive management at creating a better day for both ADHD student and teacher.
Potential Disciplinary Methods
Before implementing any of the ideas or methods listed below, a teacher should check with the school principal or school district on their policies concerning any guidelines or regulations pertaining to discipline or punishment. That said, here are some methods that can serve as forms of punishment for student misbehavior.
- Use mild, private, brief, direct reprimands – and personalize that information. That means, go to the child, touch them on the arm or shoulder, make a brief corrective statement or instruction, and have the student repeat it back. Direct, personalized instructions or reprimands are far more effective than anonymous ones given to a class as a whole or ones yelled across a room at a student.
- Immediacy is the key to discipline: Swift justice! What makes punishment work is not so much its severity or the degree of pain or unpleasantness afflicted, but the speed with which it is implemented following some misbehavior. By acting quickly following the initial occurrence of a problem, you gain credibility and will be far more effective in reducing the next occurrence of the same or similar misbehavior.
- Instead of traditional time out, try the “Do A Task” procedure. In place of the ADHD student sitting idly in a time out chair, which is an invitation to get bored and further misbehavior, this procedure gives the student something active to be done during time out. It also lets the child have some control over the length of the time out by how quickly they get the task done. Of course, all this is explained to the student beforehand so they understand what you are about to do.
- Place a vacant desk and chair at the back of the classroom with simple worksheets stacked on it.
- When a child misbehaves, tell them what they did wrong and give them a number (e.g., You yelled out in class, give me two.).
- The child then goes to the desk at the back of the class, takes a seat and does that number of worksheets as part of being timed out.
- When that work is done, the student places it on the teacher’s desk and returns to their normal seat.
- Response Cost – This simply involves a loss of tokens or loss of a privilege contingent on the student’s misbehavior. As you were cautioned earlier, however, don’t get carried away with this sort of punishment or it will ruin any incentive programs you have implemented. If loss of rewards is exceeding earned rewards, the program will lose any motivating value to that student and so become ineffective.
- Moral essays – Writing an essay concerning a rule infraction has been used for centuries as a form of discipline in school settings. Have the child write “Why I should not have … (e.g. hit other children) and what I should have done instead.” Research shows it does work, mainly for older students, but may not be as effective as other methods discussed here.
- Establish a quiet “chill out” location where an upset or misbehaving child can be sent for a brief period of isolation from the other students. The purpose of this location is to permit the child the time and a place for regaining emotional control when the child is upset.
- Use formal time outs in class or a private room – If you plan to use a time out method, remember to institute it swiftly, within seconds of a rule infraction or misbehavior. Be sure the time out location is within the classroom or in an adjoining private room that can be supervised or observed. Research shows that hallway time outs don’t work24
- For more serious or repeated forms of misconduct, consider the use of an in-school suspension or even brief placement in a Behavior Disability class.
Tips for Teen Management
Some of what follows has already been discussed above for children with ADHD. But other methods here have been developed specifically for use with teens with ADHD in school settings.
- Consider using an ADHD medication in combination with these and any of the above methods for teens. (If needed, suggest that the teen’s parent pay the teen a fee each day for complying.) Middle school and high school place far higher demands on students with ADHD for self-organization, time management, self-monitoring, and other executive functions in daily life. These stages of education also have the student interacting with more teachers and other school staff and students, often with much less structure and supervision than were provided in elementary school. For all of these reasons, ADHD medication may be needed to help with ADHD symptom control throughout the school day and to improve school functioning beyond just the behavioral methods reviewed here. The combination of treatments is far more likely to lead to a successful educational experience for the ADHD student than will either approach alone.
- Find an adult “Coach” or “Mentor” at school among the teachers or staff who will give 15 minutes a day to help the teen. This person provides three accountability checkups of the student across each school day. In short, it works like this:
- The Coach’s office is the student’s “locker.” This is where the teen goes first thing in the morning, at lunch, after school, and even between some classes rather than going to a locker.
- The Coach schedules a minimum of three five-minute checkups across each school day.
- The teen is to go to their Coach at those times for review of the school day, help with staying organized, monitoring homework assignments on an assignment sheet, tracking the student’s behavior through a daily behavior report card, and giving the student a motivational pep talk to get through to the next checkup.
- So, for example, at the start of the day, the student checks in with the Coach, gets a new behavior report card, gets a homework assignment recording sheet (if they are not using a calendar and day planner for this purpose), gets their books organized for the upcoming classes before lunch, and gets a motivational pep talk.
- At lunch, the teen returns to visit the Coach. The Coach inspects and discusses what is on the behavior report card from the morning’s teacher evaluations. The Coach also reviews the homework assignment sheet. Then the Coach helps the student organize their books and materials for the upcoming classes and gives encouragement for the afternoon classes.
- The student checks in with the Coach at the end of the school day for a review of the behavior report card, the assignment sheet, help with organizing materials that need to go home to do homework, and any further discussion of issues that arose across the day.
- Even if a Coach is not being utilized, students with ADHD can still benefit from using daily assignment sheets for recording homework.
- The teen can also benefit from using a daily or weekly school behavior card, as covered above. When the student can go for two weeks with no negative ratings, then you can move to using the card as a form of self-evaluation as discussed in an earlier chapter.
- Have the teen keep an extra set of books at home should they forget the necessary textbooks for a homework assignment that night. Parents can leave a deposit with the school office for these extra books and return them for a refund of that deposit at the end of the year.
- Again, let ADHD teens use typing/keyboard skills for written assignments rather than cursive writing, if handwriting is a problem for the teen, as it can be for many of them.
- Allow the teen to digitally record lectures so they can listen to it later when studying. Check out the Smart Pen that does this (Figure 9) at livescribe.com. The Smart Pen is a computer in a pen that helps you never miss a word™. The Pulse™ technology recording tablet helps students to record everything they hear, say and write, and links the audio recordings to their notes. Students can find the most important information from lectures just by tapping on what they wrote. The pen has 2GB of memory and can hold over 200 hours of audio recording (Of course, the actual recording time varies by audio quality setting.)
Figure 9. Smart Pen
- Ask parents to implement the “Bucks for Bs” system: Simply stated, parents pay their teenager for the grades they bring home on any assignment or exam. Teens love money so this is a great incentive for doing better at school. For instance, for every paper brought home with a grade of C, parents add $.25 to the teen’s allowance; for every grade of B, add $.50, and for every A add $1. Of course, this assumes parents have such expendable income. If they are already paying the teen an allowance, then surely they can re-align that allowance with a program like this one to reward improved schoolwork.
- Remember to schedule harder classes in late morning or early afternoon hours. Once teens enters puberty, they are not on the same wake-arousal (diurnal rhythm) cycle as children. Teens are likely to find that they are more alert later in the morning rather than first thing upon arrival at school. So keep this in mind when scheduling classes for a teen with ADHD.
- Alternate required or difficult classes with elective or more enjoyable classes across the day where possible.
- Don’t give much, if any, extra time on timed tests – there is little or no evidence it helps ADHD cases specifically; everyone benefits from a little extra time, such as X extra minutes to do a test. But it is better to have a teen with ADHD take the test in a distraction-free test setting and to employ a method called “time off the clock.” This involves using a stopwatch placed on the student’s desk. The student is permitted the same length of time “on the clock” for testing as other students. But at any time the student can stop the stopwatch, take a brief break (minute or two of stretching, getting a drink of water, etc.), after which they return to the test and restart the stopwatch. The student can do this as often as they feel a need to do so during the test. This will result in extra time being given to that student with ADHD as a byproduct of the method. But the granting of extra time is not the solution here nor is it the key ingredient. It is the breaking up of the test into shorter chunks of work and letting the teen have frequent breaks and thus self-pace the exam.
- Permit teens to listen to music via ear-buds or earphones at a quiet or reasonable level of volume while doing deskwork, studying, or during homework. Research shows this benefits attention and productivity while working compared to silent study or work periods.
- Give the teen a written syllabus as a handout to review and study for each class.
- As discussed above for children, require that the teen with ADHD engage in note-taking in class and while reading to help them to pay attention.25
- Teach the teen this simple “SQ4R” system to boost reading comprehension while studying or doing homework:26
- Survey the assigned material.
- Review or draft Questions to be answered, then for each paragraph:
- Read it,
- Recite what is important to remember,
- wRite it down, and then
- Review what was written.
- Do this again after each new paragraph.
- Try peer tutoring in class for teens (see Peer Tutoring above).
- “Study-with-a-buddy” after school (see above).
- Find “fall-back” classmates: with these students, swap phone, e-mail, and fax numbers to contact them for lost or missing assignment sheets.
- Require the teen to attend after-school help sessions whenever available or to get some scheduled if they are not routinely offered to students. If motivation to do so is a problem for the teen with ADHD, see if the parents can institute a financial reward for doing so, as in the Bucks for Bs system noted above.
- Schedule parent-teacher review meetings with teen every six weeks (rather than at the nine-week grading period).
Medications Used to Manage ADHD
Between 40% and 80% of children and teens with ADHD are likely to be taking an ADHD medication as part of their treatment by a physician. It is therefore helpful for educators to know the types of medications their students with ADHD are likely to be taking, how the drugs work, and what the side effects are likely to be. Children taking medication are likely to be more responsive to the behavioral methods used to manage ADHD-related school problems and the combination of those methods with medication often results in far greater improvement than when either form of treatment is used alone.
For more information on medications, see my course ADHD in Children: Diagnosis, Assessment, and Management. There are three basic categories of ADHD medicines that are approved by the Food and Drug Administration for use with children and teens – stimulants, non-stimulants, and anti-hypertensive drugs. All have to be taken daily. They all control the symptoms of ADHD only as long as your student takes the medications. They produce no enduring positive effects on your student’s ADHD if they stop taking them. Ceasing the use of medication often results in a return of the ADHD symptoms back to their pre-treatment levels. Think of these medicines as you would insulin with a diabetic. Insulin does not cure diabetes, but it does manage it so long as it is used, and if used properly, for most people. But if your student stops the medication the underlying problem and its symptoms will return.
The first two types of ADHD medications typically work by increasing the amount of two (or more) chemicals in the brain known as neurotransmitters. Those chemicals are involved in permitting nerve cells to communicate with each other so the brain can function effectively. More specifically, these drugs increase just how much of these chemicals are residing outside of the nerve cells. That can increase the activity of adjacent nerve cells. The two neurotransmitters are dopamine and norepinephrine. By causing nerve cells to express more of these neurochemicals, or by keeping the nerve cells from pulling these chemicals back into the cell once they have been released, they increase the communication that occurs between nerve cells in regions of the brain that are related to directly causing ADHD. In short, increasing these brain chemicals in these regions lets that brain area function better, and sometimes even normally. Also, recent studies show that children who have taken these medications (especially the stimulants) are likely to have brain development that is closer to normal than children with ADHD who have not taken the medication – a phenomenon known as neuroprotection. The third class of medications works by fine tuning small ports on the nerve cells mainly in the frontal cortex. In doing so, they strengthen the balance of nerve signals to noise within the nerve cell allowing the cell to be more likely to function properly.
Types of Stimulants and their Actions
There are two basic types of stimulants currently marketed in the U.S. – methylphenidate (MPH) and amphetamine (AMP). These stimulants act in the brain to mainly increase the amount of dopamine available for use outside the nerve cells. Yet they can, to a smaller extent, increase the amount of norepinephrine outside the nerve cells as well. AMP does this mainly by increasing the amount of dopamine that is produced and expressed from the nerve cell when it is activated. To a lesser extent, it may also block the transport system by which the dopamine is normally re-absorbed back into that nerve cell after being released. That can result in more dopamine being left outside the cell to continue to function. MPH mainly acts by preventing this re-absorption of dopamine. That is why it is known as a transport or re-uptake blocker.
Both AMP and MPH have the potential to be abused because they increase dopamine in regions of the brain known as reward centers. Stimulating those centers can lead to an increased likelihood of addiction to drugs that do so. But ADHD medications are very unlikely to do this when taken by mouth and swallowed, as prescribed. They certainly can do so when they are sniffed through the nose as a powder or injected into a blood vein in a solution, such as when mixed with water. Because of this potential for drug abuse, the Drug Enforcement Administration in the U.S. has classified these stimulants as Schedule II Controlled Substances along with other potentially addictive drugs. This classification places limits on how much of the drugs can be produced annually, how the drugs are to be prescribed, how they are to be stored in pharmacies, and how they are to be dispensed and otherwise monitored in the U.S.
There are many different methods by which these two drugs are delivered into the body. The major methods are described in the Box below. The methods differ in how long they maintain the blood levels of the drug in the body, and so in the brain. There are hundreds of studies on the safety and effectiveness of these stimulants and delivery systems.
|
The different delivery systems are the 5 Ps – pills, pumps, pellets, patches, and pro-drug along with the delayed onset-extended release method (Jornay PM), and the liquid extended release and gummy (oral dissolvable) sustained release methods. The various brand names of ADHD medicines you will hear about are either one form or another of MPH or AMP and involve one of these delivery systems:
|
Side Effects of Stimulants
The most common side effects people experience when taking a stimulant (MPH or AMP) are listed below in their descending order of likely occurrence:
- Insomnia, or trouble falling asleep
- Loss of appetite, especially for the mid-day meal (some adults perceive this as a benefit if they are trying to lose weight)
- Weight loss (again some adults do not see this as an adverse effect but a positive effect if they are trying to lose weight)
- Headaches
- Nausea, upset stomach, or stomachache
- Anxiety (the research is somewhat mixed on whether stimulants worsen anxiety but enough studies have found this to be the case, particularly with children with ADHD, that it should continue to be listed as a possible adverse effect)
- Irritability, or being easily upset, angered, or prone to outbursts. But just as often or more often, managing the ADHD can actually reduce problems with controlling one’s emotions. As we saw earlier, problems with regulating one’s emotions actually goes with ADHD, so treating the ADHD can often make this area of functioning better, not worse.
- Motor tics; stimulants may not cause these outright in patients unless they have a family history for tic disorders and thus are somewhat more vulnerable to develop a tic than are others without such a history. If tics are already present, they can be worsened in up to 1/3 of such cases, but in the remainder the tics remain unchanged or may even be improved. AMP is more likely to provoke tic reactions than is MPH.
- Increased muscle tension. Though not very common, some people report sensations like those they may have if they drink too much caffeine, including tenseness of or frequent clenching of the jaw, muscle tension in the forehead, or generally feeling more taut in their posture.
These stimulants also increase heart rate and blood pressure slightly, but generally no more so and often less so than if you had just climbed a half-flight of stairs. You may have heard claims that these drugs increase the sensitivity to or risk for abusing other drugs, especially other stimulants. The vast majority of research does not support this claim. People who have taken ADHD medications such as these stimulants for years, including children growing up with ADHD, were found to be no more likely to abuse drugs than were those not being treated. In fact, in a few studies they were found to be less likely to do so, probably because the ADHD medication was controlling their impulsiveness.
You may have also heard that these drugs, especially the stimulants, might increase the likelihood of sudden death, usually from heart block (heart stops beating). In rare cases, strokes have occurred in people taking these drugs. While some people have died while taking a stimulant, these cases always involve other extenuating factors that alone can account for the sudden death. Those reasons include things like a history of structural heart defects along with engaging in vigorous exercise just preceding the death. The available evidence actually shows that people on stimulants have a somewhat lower likelihood of sudden death than the general population (which is one to seven people per 100,000 per year, depending on age). This is probably because physicians routinely screen for heart problems before starting people on stimulants and, if discovered, usually do not use these medications. So those with the greatest likelihood of having heart problems if they took a stimulant are not prescribed them. Even so, physicians have been cautioned not to put people on stimulants if they have a history of sudden death in their family or a history of structural heart abnormalities, major arrhythmias, or other major cardiac problems. It also makes sense not to treat people with clinically or morbidly high blood pressure with a stimulant for the obvious reason that it can make the situation even more risky for them. The risk to otherwise healthy children and teens with ADHD is not significant if there is any increased risk at all.
Non-stimulants (NERIs: Norepinephrine Reuptake Inhibitors)
In 2003, the FDA approved the first non-stimulant drug for the management of child, teen, and adult ADHD, and the first new drug for ADHD in more than 25 years. That drug was Atomoxetine (ATX), under the brand name Strattera®. This was the most studied ADHD drug before receiving FDA approval that has ever been brought to market. Randomized and double-blinded studies were done involving more than 6,000 patients worldwide to thoroughly study the effectiveness, side effects, and safety of this medication. Now, like the stimulants above, millions of people worldwide take this medication for management of their ADHD. Then, in March of 2021, the FDA approved another NERI type medication – viloxazine (QelBree®), which works in a very similar way as atomoxetine.
As noted above, AMP acts in the brain by increasing the amount of dopamine that is produced and expressed from the nerve cell when it is activated. To a lesser extent, it may also block the transport system by which the dopamine is normally re-absorbed back into that nerve cell after being released. MPH mainly acts by preventing this re-absorption of dopamine and so is known as a transport or re-uptake blocker. Atomoxetine (ATX) and viloxazine (VLX), in contrast, work by blocking the re-absorption of norepinephrine once it has been released. Like, MPH, they are re-uptake blockers, but they block the re-uptake of a different neuro-chemical; that is norepinephrine. Some research shows that by doing this, both drugs probably result in an increase in dopamine outside nerve cells in certain parts of the brain, such as the frontal cortex.
These non-stimulants also differ from the stimulants, however, in that they do not affect the brain centers that are likely to be related to drug addiction or abuse. This is why the drugs are called non-stimulants. It is also why they are not classified as a controlled substances in the U.S. Research shows that the drugs have a very low potential for abuse. That means it is not preferred or liked by known drug addicts more than other psychiatric drugs such as anti-depressants, which is to say addicts like them very little. The different means by which they acts in the brain can result in a different profile of potential side effects and adverse reactions, and possibly somewhat different benefits from these drugs than what one sees with the stimulants.
The non-stimulants are nearly as effective for managing ADHD symptoms as is MPH, but not quite as effective as AMP, the most powerful of the prescribed stimulants. The same percentage of patients appears to positively respond to both these classes of drugs (stimulants and non-stimulants), averaging about 75% of people responding to any single drug. However, some studies suggest that while 50% of people respond positively to both types of medications, 25% may respond better to a stimulant than to a non-stimulant while the remaining 25% may respond better to non-stimulants than to one of the stimulants. In other words, some people are unique responders who do better on one type of ADHD drug than on another. We should not be surprised at this given that not all people are biologically identical especially in the organization and functioning of their brains. Some studies suggest that non-stimulants may not produce quite as much improvement in ADHD symptoms as do the stimulants while others show they are at least equivalent to MPH. But for many children, the degree of improvement is sufficient to effectively manage their disorder while not necessarily producing the same types of side effects that one might get with a stimulant. Also, stimulants have the potential to be abused or diverted for such abuse to others who were not prescribed the drug. Non-stimulants do not adversely affect anxiety, may even reduce it significantly, do not worsen tics or nervous habits, and do not typically result in insomnia.
The issue that physicians face in daily practice with ADHD patients is therefore not which drug works better, but which drug is best suited to which individual patient given their unique profile of characteristics. Having many different drugs, just like having many different delivery systems, lets physicians better tailor their treatment to the uniqueness of each patient. Your student can expect, however, that with a non-stimulant, it will take longer to adjust it to the right dosage than is the case with a stimulant. That is because it takes longer for the body to adjust to the side effects of NERI drugs like ATX. And that is why physicians like to leave patients on a particular dosage a week or two longer than they might with a stimulant before adjusting the dosage upward.
Side Effects of NERI Non-stimulants
The most common side effects for NERI drugs are:
- Nausea or vomiting
- Dry mouth
-
- Dizziness or light-headedness
- Constipation
- Sweating
- Decreased libido (sex drive) or erectile dysfunction
- Sweating
- Insomnia (far less common than with stimulants)
- Irritability (same as with stimulants – some patients actually report improvement in their mood or emotional self-control while on this medication)
Although non-stimulants can also increase heart rate and blood pressure, they do so less than the stimulants discussed above. There is an exceptionally rare chance of liver complications that occur once in every 2 million people treated with ATX (two cases out of 4.5 million treated to date; and one of these is arguable). This seems to result from a very rare auto-immune reaction to the drug in which the body’s immune system attacks and inflames the outer layers of the liver. So the risk for this side effect is incredibly low. No evidence has yet accumulated on the latest NERI drug, VLX, to say if it creates this same problem but given its chemical similarity, that remains a possibility. So to be safe, people with a history of liver damage or other liver problems may want to avoid using NERI drugs like ATX.
The package inserts for the non-stimulants contain a warning of a possibility of increased suicidal thinking from this drug, but not suicide attempts, and this increase in ideation was seen only in children. This side effect is highly questionable given the lack of rigor with which the information on which it is based was collected in the initial clinical trials for this drug. This problem of increased suicidal thinking was not found for teens and adults with ADHD taking ATX. Also, more recent large-scale research has found that people with ADHD who are off medication have a far higher rate of suicidal thinking and attempts than do those who are taking either ATX or a stimulant medication. These findings suggest that taking these medicines for ADHD may actually reduce the risk for suicidal thinking and attempts.
Anti-Hypertensive (Alpha-2) Drugs
Two other medicines are sometimes used to treat adult ADHD, but they should be considered “last choice” medicines to be used only if the other ADHD medicines are not proving satisfactory. Both originated as drugs used to treat high blood pressure, called anti-hypertensive drugs. One is clonidine, and works as an alpha-adrenergic enhancer. Some nerve cells in the brain have little portholes on them called alpha-2 receptors. These drugs seem to act to reduce or close off these portholes and that results in stronger or more effective nerve signals in those cells. At low dosages, this drug appears to stimulate inhibitory systems in the brain. The FDA approved an extended-release version of clonidine, clonidine ER (Kapvay®), in 2010 as a treatment for ADHD in children ages 6-17 years. But as noted above, physicians can use it “off-label” outside of this age range, such as for adults with ADHD. It can be used alone or combined with stimulants. The drug is not as effective as the other ADHD medicines discussed above. So it is sometimes used to treat ADHD when it co-exists with other disorders such as conduct or antisocial problems or irritability and anger. It can also treat tic disorders, sleep disturbances, and may reduce anxiety.
Regular clonidine is fast-acting. But the extended-release version approved for ADHD can last much longer. The most common side effect of clonidine is sedation, which tends to subside with continued treatment. It can also result in reduced blood pressure, called hypotension, and sometimes results in complaints of dry mouth, vivid dreams, depression, and confusion. Unlike other ADHD medicines, this one cannot be stopped abruptly. It requires slow tapering over several days to weeks. The drug should not be used if your student is taking beta-blockers or calcium channel blockers. Experts recommend that anyone using these drugs for treating ADHD have their blood pressure monitored when starting or when tapering off clonidine and when dosages are being increased.
Another anti-hypertensive drug used for ADHD management is guanfacine. In 2009, the FDA approved an extended-release version, guanfacine ER (Intuniv®) for the treatment of ADHD in people 6-17 years of age. Again, physicians can use it with adults off-label if they think it essential to do so. The drug can be given alone or in combination with either of the stimulant medicines discussed above, as monotherapy, or as adjunctive treatment with stimulants.
There may be some advantages of guanfacine over clonidine. These include less sedation, a longer duration of action, and less risk of cardiovascular problems.
This drug can result in minor decreases in blood pressure and pulse rate. Other side effects include sedation, irritability, and depression. Again, this medication probably is not as effective as the stimulants or ATX discussed above. Its benefit may be in helping to treat coexisting disorders with ADHD, such as anger and aggression, and in reducing highly impulsive or hyperactive behavior.
You and your student should be aware that there is very little research on using these two anti-hypertensive drugs to treat ADHD in adults. That is why they were FDA approved mainly for children, on which more research was available. Because of the lack of research, these drugs are considered last choice options for managing adult ADHD. The other ADHD medicines above should be tried first.
Conclusion
-
The management of ADHD in educational settings requires as a prerequisite that mental health professionals be knowledgeable about the nature of the disorder, its symptoms, the deficits in executive functioning associated with it (both cognitive and in daily adaptive functioning), as well as its demographics and etiologies. With this information in mind, especially the nature of the EF deficits inherent in ADHD, professionals can proceed to tailor a suite of intervention methods for a specific child or teen from a wide array of more than 80 methods of behavior management and classroom accommodation. All of these methods are grounded in a set of 10 overarching principles of management which themselves are grounded in the nature of EF and its deficits in ADHD.
